Liposomal amphotericin B (AmBisome) efficacy in confirmed
- 格式:pdf
- 大小:76.50 KB
- 文档页数:6
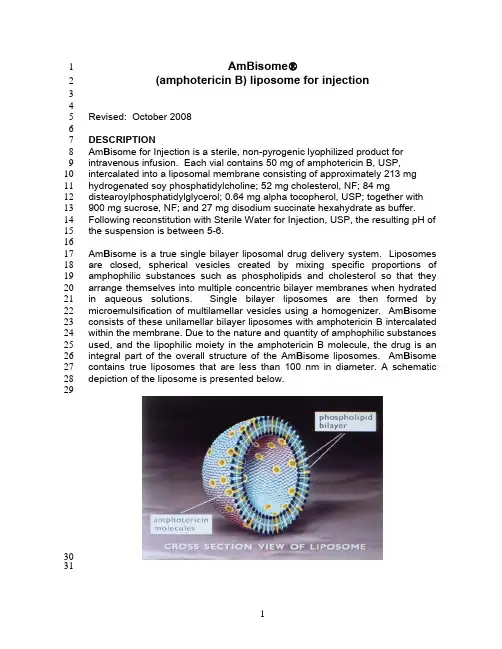
AmBisome®1(amphotericin B) liposome for injection2345Revised: October 200867DESCRIPTION8Am B isome for Injection is a sterile, non-pyrogenic lyophilized product for9intravenous infusion. Each vial contains 50 mg of amphotericin B, USP,intercalated into a liposomal membrane consisting of approximately 213 mg1011hydrogenated soy phosphatidylcholine; 52 mg cholesterol, NF; 84 mg12distearoylphosphatidylglycerol; 0.64 mg alpha tocopherol, USP; together with13900 mg sucrose, NF; and 27 mg disodium succinate hexahydrate as buffer.14Following reconstitution with Sterile Water for Injection, USP, the resulting pH of 15the suspension is between 5-6.16Am B isome is a true single bilayer liposomal drug delivery system. Liposomes1718are closed, spherical vesicles created by mixing specific proportions of 19amphophilic substances such as phospholipids and cholesterol so that they 20arrange themselves into multiple concentric bilayer membranes when hydrated 21in aqueous solutions. Single bilayer liposomes are then formed by 22microemulsification of multilamellar vesicles using a homogenizer. Am B isome 23consists of these unilamellar bilayer liposomes with amphotericin B intercalated 24within the membrane. Due to the nature and quantity of amphophilic substances 25used, and the lipophilic moiety in the amphotericin B molecule, the drug is an integral part of the overall structure of the Am B isome liposomes. Am B isome2627contains true liposomes that are less than 100 nm in diameter. A schematic 28depiction of the liposome is presented below.293031Note: Liposomal encapsulation or incorporation into a lipid complex can3233substantially affect a drug’s functional properties relative to those of the34unencapsulated drug or non-lipid associated drug. In addition, differentliposomal or lipid-complex products with a common active ingredient may vary 3536from one another in the chemical composition and physical form of the lipid37component. Such differences may affect the functional properties of these drug38products.3940Amphotericin B is a macrocyclic, polyene, antifungal antibiotic produced from a41strain of Streptomyces nodosus. Amphotericin B is designated chemically as:[1R-(1R*,3S*,5R*,6R*,9R*,11R*,15S*,16R*,17R*,18S*,424319E,21E,23E,25E,27E,29E,31E,33R*,35S*,36R*,37S*)]-33-[(3-Amino-3,6-44dideoxy-β-D-mannopyranosyl)oxy]-1,3,5,6,9,11,17,37-octahydroxy-15,16,18-45trimethyl-13-oxo-14,39-dioxabicyclo[33.3.1]nonatriaconta-19,21,23,25,27,29,31-46heptaene-36-carboxylic acid (CAS No. 1397-89-3).47Amphotericin B has a molecular formula of C47H73NO17 and a molecular weight4849of 924.09.5051The structure of amphotericin B is shown below:5253545556MICROBIOLOGY57Mechanism of Action58Amphotericin B, the active ingredient of Am B isome, acts by binding to the sterol59component of a cell membrane leading to alterations in cell permeability and60cell death. While amphotericin B has a higher affinity for the ergosterol61component of the fungal cell membrane, it can also bind to the cholesterol 62component of the mammalian cell leading to cytotoxicity. Am B isome, the63liposomal preparation of amphotericin B, has been shown to penetrate the cell64wall of both extracellular and intracellular forms of susceptible fungi.6566Activity In Vitro and In Vivo67Am B isome has shown in vitro activity comparable to amphotericin B against the68following organisms: Aspergillus species (A. fumigatus, A. flavus), Candida69species (C. albicans, C. krusei, C. lusitaniae, C. parapsilosis, C. tropicalis),70Cryptococcus neoformans, and Blastomyces dermatitidis. However,71standardized techniques for susceptibility testing of antifungal agents have not72been established and results of such studies do not necessarily correlate with 73clinical outcome.7475Am B isome is active in animal models against Aspergillus fumigatus,Candida 76albicans, Candida krusei, Candida lusitaniae, Cryptococcus neoformans, Blastomyces dermatitidis, Coccidioides immitis, Histoplasma capsulatum,7778Paracoccidioides brasiliensis, Leishmania donovani, and Leishmania infantum.79The administration of Am B isome in these animal models demonstrated 80prolonged survival of infected animals, reduction of microorganisms from target 81organs, or a decrease in lung weight.8283Drug ResistanceMutants with decreased susceptibility to amphotericin B have been isolated8485from several fungal species after serial passage in culture media containing the 86drug, and from some patients receiving prolonged therapy. Drug combination 87studies in vitro and in vivo suggest that imidazoles may induce resistance to 88amphotericin B. However, the clinical relevance of drug resistance has not 89been established.9091CLINICAL PHARMACOLOGY92PharmacokineticsThe assay used to measure amphotericin B in the serum after administration of9394Am B isome does not distinguish amphotericin B that is complexed with the95phospholipids of Am B isome from amphotericin B that is uncomplexed. The96pharmacokinetic profile of amphotericin B after administration of Am B isome is 97based upon total serum concentrations of amphotericin B. The 98pharmacokinetic profile of amphotericin B was determined in febrile neutropenic cancer and bone marrow transplant patients who received 1-2 hour infusions of 991001 to 5 mg/kg/day Am B isome for 3 to 20 days.The pharmacokinetics of amphotericin B after administration of Am B isome are 101102nonlinear such that there is a greater than proportional increase in serum 103concentrations with an increase in dose from 1 to 5 mg/kg/day. The 104pharmacokinetic parameters of total amphotericin B (mean ± SD) after the first dose and at steady state are shown in the table below.105106Pharmacokinetic Parameters of AmBisome Dose (mg/kg/day):1 2.5 5 Day 1 n = 8 Last n = 7 1 n = 7 Last n = 7 1 n = 12 Lastn = 9ParametersC max (mcg/mL)7.3 ± 3.8 12.2 ± 4.9 17.2 ± 7.1 31.4 ± 17.8 57.6 ± 21 83 ± 35.2 AUC 0-24 (mcg •hr/mL)27 ± 14 60 ± 20 65 ± 33 197 ± 183 269 ± 96 555 ± 311 t ½(hr) 10.7 ± 6.4 7 ± 2.1 8.1 ± 2.3 6.3 ± 2 6.4 ± 2.1 6.8 ± 2.1 V ss (L/kg) 0.44 ± 0.27 0.14 ± 0.05 0.40 ± 0.37 0.16 ± 0.09 0.16 ± 0.10 0.10 ± 0.07 Cl (mL/hr/kg) 39 ± 22 17 ± 6 51 ± 44 22 ± 15 21 ± 14 11 ± 6 107Distribution 108Based on total amphotericin B concentrations measured within a dosing interval 109(24 hours) after administration of Am B isome, the mean half-life was 7-10 hours. 110However, based on total amphotericin B concentration measured up to 49 days 111after dosing of Am B isome, the mean half-life was 100-153 hours. The long 112terminal elimination half-life is probably a slow redistribution from tissues. 113Steady state concentrations were generally achieved within 4 days of dosing. 114115Although variable, mean trough concentrations of amphotericin B remained 116relatively constant with repeated administration of the same dose over the 117range of 1 to 5 mg/kg/day, indicating no significant drug accumulation in the 118serum. 119120Metabolism 121The metabolic pathways of amphotericin B after administration of Am B isome 122are not known. 123124Excretion 125The mean clearance at steady state was independent of dose. The excretion of 126amphotericin B after administration of Am B isome has not been studied. 127128Pharmacokinetics in Special Populations 129Renal Impairment 130The effect of renal impairment on the disposition of amphotericin B after 131administration of Am B isome has not been studied. However, Am B isome has 132been successfully administered to patients with pre-existing renal impairment 133(see DESCRIPTION OF CLINICAL STUDIES ). 134135Hepatic Impairment 136The effect of hepatic impairment on the disposition of amphotericin B after 137administration of Am B isome is not known. 138139Pediatric and Elderly Patients 140The pharmacokinetics of amphotericin B after administration of Am B isome in 141pediatric and elderly patients have not been studied; however, Am B isome has 142been used in pediatric and elderly patients (see DESCRIPTION OF CLINICAL 143STUDIES ). 144145Gender and Ethnicity 146The effect of gender or ethnicity on the pharmacokinetics of amphotericin B 147after administration of Am B isome is not known. 148149INDICATIONS AND USAGE 150Am B isome is indicated for the following: 151152• Empirical therapy for presumed fungal infection in febrile, neutropenic 153patients. 154• Treatment of Cryptococcal Meningitis in HIV infected patients (see 155DESCRIPTION OF CLINICAL STUDIES ). 156• Treatment of patients with Aspergillus species, Candida species and/or 157Cryptococcus species infections (see above for the treatment of 158Cryptococcal Meningitis) refractory to amphotericin B deoxycholate, or in 159patients where renal impairment or unacceptable toxicity precludes the use 160of amphotericin B deoxycholate. 161• Treatment of visceral leishmaniasis. In immunocompromised patients with 162visceral leishmaniasis treated with Am B isome, relapse rates were high 163following initial clearance of parasites (see DESCRIPTION OF CLINICAL 164STUDIES ). 165166See DOSAGE AND ADMINISTRATION for recommended doses by indication. 167168DESCRIPTION OF CLINICAL STUDIES 169Eleven clinical studies supporting the efficacy and safety of Am B isome were 170conducted. This clinical program included both controlled and uncontrolled 171studies . These studies, which involved 2171 patients, included patients with 172confirmed systemic mycoses, empirical therapy, and visceral leishmaniasis. 173174Nineteen hundred and forty-six episodes were evaluable for efficacy, of which 1751280 (302 pediatric and 978 adults) were treated with Am B isome. 176177Three controlled empirical therapy trials compared the efficacy and safety of 178Am B isome to amphotericin B. One of these studies was conducted in a 179pediatric population, one in adults, and a third in patients aged 2 years or more. 180In addition, a controlled empirical therapy trial comparing the safety of 181Am B isome to Abelcet ® (amphotericin B lipid complex) was conducted in 182patients aged 2 years or more. 183184185One controlled trial compared the efficacy and safety of Am B isome to186amphotericin B in HIV patients with cryptococcal meningitis.187188One compassionate use study enrolled patients who had failed amphotericin B189deoxycholate therapy or who were unable to receive amphotericin B190deoxycholate because of renal insufficiency.191192Empirical Therapy in Febrile Neutropenic PatientsStudy 94-0-002, a randomized, double-blind, comparative multi-center trial,193194evaluated the efficacy of Am B isome (1.5-6 mg/kg/day) compared with195amphotericin B deoxycholate (0.3-1.2 mg/kg/day) in the empirical treatment of196687 adult and pediatric neutropenic patients who were febrile despite having197received at least 96 hours of broad spectrum antibacterial therapy. Therapeutic198success required (a) resolution of fever during the neutropenic period, (b)199absence of an emergent fungal infection, (c) patient survival for at least 7 days200post therapy, (d) no discontinuation of therapy due to toxicity or lack of efficacy,201and (e) resolution of any study-entry fungal infection.202203The overall therapeutic success rates for Am B isome and the amphotericin B204deoxycholate were equivalent. Results are summarized in the following table.205Note: The categories presented below are not mutually exclusive.206Empirical Therapy in Febrile Neutropenic Patients:Randomized, Double-Blind Study in 687 PatientsBAmphotericin AmBisome343 344Number of patients receiving at least onedose of study drugOverall Success 171 (49.9%) 169 (49.1%)199 (58%) 200 (58.1%)Fever resolution duringneutropenic periodNo treatment emergent fungal infection 300 (87.5%) 301 (87.7%)318 (92.7%) 308 (89.5%)Survival through 7 days poststudy drugStudy drug not prematurelydiscontinued due to toxicity294 (85.7%) 280 (81.4%)or lack of efficacy*207* 8 and 10 patients, respectively, were treated as failures due to premature discontinuation208alone.209210This therapeutic equivalence had no apparent relationship to the use of211prestudy antifungal prophylaxis or concomitant granulocytic colony stimulating212factors.213The incidence of mycologically confirmed and clinically diagnosed, emergent214215fungal infections are presented in the following table. Am B isome and216amphotericin B were found to be equivalent with respect to the total number ofemergent fungal infections.217218Empirical Therapy in Febrile Neutropenic Patients:Emergent Fungal InfectionsBAmBisome Amphotericin343 344 Number of patients receiving at leastone dose of study drug11 (3.2%) 27 (7.8%)Mycologically confirmed fungalinfection32 (9.3%) 16 (4.7%)Clinically diagnosed fungalinfection43 (12.5%) 43 (12.5%)Total emergentfungal infections219220Mycologically confirmed fungal infections at study-entry were cured in 8 of 11221patients in the Am B isome group and 7 of 10 in the amphotericin B group.222223Study 97-0-034, a randomized, double-blind, comparative multi-center trial,224evaluated the safety of Am B isome (3 and 5 mg/kg/day) compared with 225amphotericin B lipid complex (5 mg/kg/day) in the empirical treatment of 202 226adult and 42 pediatric neutropenic patients. One hundred and sixty-six patients227received Am B isome (85 patients received 3 mg/kg/day and 81 received 5 mg/kg/day) and 78 patients received amphotericin B lipid complex. The study 228229patients were febrile despite having received at least 72 hours of broad 230spectrum antibacterial therapy. The primary endpoint of this study was safety.The study was not designed to draw statistically meaningful conclusions related 231232to comparative efficacy, and in fact, Abelcet is not labeled for this indication.233Two supportive prospective randomized, open label, comparative multi-center 234235studies examined the efficacy of two dosages of Am B isome (1 and 3 236mg/kg/day) compared to amphotericin B deoxycholate (1 mg/kg/day) in the 237treatment of neutropenic patients with presumed fungal infections. These 238patients were undergoing chemotherapy as part of a bone marrow transplant or 239had hematological disease. Study 104-10 enrolled adult patients (n=134).Study 104-14 enrolled pediatric patients (n=214). Both studies support the 240241efficacy equivalence of Am B isome and amphotericin B as empirical therapy in 242febrile neutropenic patients.243244Treatment of Cryptococcal Meningitis in HIV Infected Patients.245Study 94-0-013, a randomized, double-blind, comparative multi-center trial,evaluated the efficacy of Am B isome at doses ( 3 and 6 mg/kg/day) compared 246247with amphotericin B deoxycholate (0.7 mg/kg/day) for the treatment of 248cryptococcal meningitis in 266 adult and one pediatric HIV positive patients (the pediatric patient received amphotericin B deoxycholate). Of the 267 treated 249patients, 86 received Am B isome 3 mg/kg/day, 94 received 6 mg/kg/day and 87 250received amphotericin B deoxycholate; cryptococcal meningitis was 251252documented by a positive CSF culture at baseline in 73, 85 and 76 patients, 253respectively. Patients received study drug once daily for an induction period of11 to 21 days. Following induction, all patients were switched to oral 254255fluconazole at 400 mg/day for adults and 200 mg/day for patients less than 13years of age to complete 10 weeks of protocol-directed therapy. For 256mycologically evaluable patients, defined as all randomized patients who 257received at least one dose of study drug, had a positive baseline CSF culture, 258and had at least one follow-up culture, success was evaluated at week 2 (i.e., 25914 ± 4 days), and was defined as CSF culture conversion. Success rates at 2 260weeks for Am B isome and amphotericin B deoxycholate are summarized in the 261following table:262263Success Rates at 2 weeks (CSF Culture Conversion) Study 94-0-013264AmBisome 3 mg/kg AmBisome6 mg/kgAmphotericin B0.7 mg/kgSuccess at Week 235/60 (58.3%)97.5% CI1= -9.4%,+31%36/75(48%) 97.5% CI1=-18.8%, +19.8%29/61 (47.5 %)2651 97.5% Confidence Interval for the difference between Am B isome and amphotericin B 266success rates. A negative value is in favor of amphotericin B. A positive value is in 267favor of Am B isome.268269Success at 10 weeks was defined as clinical success at week 10 plus CSF 270culture conversion at or prior to week 10. Success rates at 10 weeks in patients 271with positive baseline culture for cryptococcus species are summarized in the 272following table and show that the efficacy of Am B isome 6 mg/kg/day 273approximates the efficacy of the amphotericin B deoxycholate regimen. These 274data do not support the conclusion that Am B isome 3 mg/kg/day is comparable 275in efficacy to amphotericin B deoxycholate. The table also presents 10-week 276survival rates for patients treated in this study.277278279Success Rates and Survival Rates at week 10, Study 94-0-013280(see text for definitions)281AmBisome 3 mg/kg AmBisome6 mg/kgAmphotericin B0.7 mg/kgSuccess in patients with documented cryptococcal meningitis27/73 (37%)97.5% CI1=-33.7%, +2.4%42/85 (49%)97.5% CI1=-20.9%, 14.5%40/76 (53%)Survival rates74/86 (86%)97.5% CI1=-13.8%, +8.9%85/94 (90%)97.5% CI1=-8.3%, +12.2%77/87 (89%)2821 97.5% Confidence Interval for the difference between Am B isome and amphotericin B 283rates. A negative value is in favor of amphotericin B. A positive value is in favor of 284Am B isome.285286The incidence of infusion-related, cardiovascular and renal adverse events was 287lower in patients receiving Am B isome compared to amphotericin B 288deoxycholate (see ADVERSE REACTIONS section for details), therefore, the 289risks and benefits (advantages and disadvantages) of the different amphotericin 290B formulations should be taken into consideration when selecting a patient 291treatment regimen.292293Treatment of Patients with Aspergillus Species, Candida Species and/or 294Cryptococcus Species Infections Refractory to Amphotericin B 295Deoxycholate, or in Patients Where Renal Impairment or Unacceptable 296Toxicity Precludes the Use of Amphotericin B Deoxycholate297Am B isome was evaluated in a compassionate use study in hospitalized patients 298with systemic fungal infections. These patients either had fungal infections 299refractory to amphotericin B deoxycholate, were intolerant to the use of 300amphotericin B deoxycholate, or had pre-existing renal insufficiency. Patient 301recruitment involved 140 infectious episodes in 133 patients, with 53 episodes 302evaluable for mycological response and 91 episodes evaluable for clinical 303outcome. Clinical success and mycological eradication occurred in some 304patients with documented aspergillosis, candidiasis, and cryptococcosis.305306Treatment of Visceral Leishmaniasis307Am B isome was studied in patients with visceral leishmaniasis who were 308infected in the Mediterranean basin with documented or presumed Leishmania 309infantum. Clinical studies have not provided conclusive data regarding efficacy 310against L. donovani or L. chagasi.311312Am B isome achieved high rates of acute parasite clearance in 313immunocompetent patients when total doses of 12-30 mg/kg were 314administered. Most of these immunocompetent patients remained relapse-free 315during follow-up periods of 6 months or longer. While acute parasite clearance 316was achieved in most of the immunocompromised patients who received total 317doses of 30-40 mg/kg, the majority of these patients were observed to relapse 318in the 6 months following the completion of therapy. Of the 21 319immunocompromised patients studied, 17 were coinfected with HIV; 320approximately half of the HIV infected patients had AIDS. The following table 321presents a comparison of efficacy rates among immunocompetent and 322immunocompromised patients infected in the Mediterranean basin who had no 323prior treatment or remote prior treatment for visceral leishmaniasis. Efficacy is 324expressed as both acute parasite clearance at the end of therapy (EOT) and as 325overall success (clearance with no relapse) during the follow-up period (F/U) of 326greater than 6 months for immunocompetent and immunocompromised 327patients:328329330AmBisome Efficacy in Visceral LeishmaniasisImmunocompetent PatientsNo. of Patients Parasite (%) Clearance atEOT Overall Success (%) atF/U87 86/87 (98.9) 83/86 (96.5)Immunocompromised PatientsRegimen Total Dose Parasite (%) Overall Success (%) atClearance atF/UEOT29-38.9 mg/kg 10/10 (100) 2/10 (20)100 mg/dayX 21 days4 mg/kg/day, days40 mg/kg 8/9 (88.9) 0/7 (0)1-5, and 10, 17, 24,31, 38TOTAL 18/19 (94.7) 2/17 (11.8)331332When followed for 6 months or more after treatment, the overall success rate 333among immunocompetent patients was 96.5% and the overall success rate 334among immunocompromised patients was 11.8% due to relapse in the majority 335of patients. While case reports have suggested there may be a role for long-336term therapy to prevent relapses in HIV coinfected patients (Lopez-Dupla, et al. 337J Antimicrob Chemother 1993; 32: 657-659), there are no data to date 338documenting the efficacy or safety of repeat courses of Am B isome or of 339maintenance therapy with this drug among immunocompromised patients.340CONTRAINDICATIONS341342Am B isome is contraindicated in those patients who have demonstrated or have 343known hypersensitivity to amphotericin B deoxycholate or any other constituents of the product unless, in the opinion of the treating physician, the 344345benefit of therapy outweighs the risk.346347WARNINGS348Anaphylaxis has been reported with amphotericin B deoxycholate and other amphotericin B-containing drugs, including Am B isome. If a severe anaphylactic 349350reaction occurs, the infusion should be immediately discontinued and the patient should not receive further infusions of Am B isome.351352353PRECAUTIONS354General355As with any amphotericin B-containing product the drug should be administered 356by medically trained personnel. During the initial dosing period, patients should 357be under close clinical observation. Am B isome has been shown to be 358significantly less toxic than amphotericin B deoxycholate; however, adverse 359events may still occur.360Laboratory Tests361362Patient management should include laboratory evaluation of renal, hepatic and 363hematopoietic function, and serum electrolytes (particularly magnesium and potassium).364365366Drug Interactions367No formal clinical studies of drug interactions have been conducted with 368Am B isome. However, the following drugs are known to interact with 369amphotericin B and may interact with Am B isome:370Antineoplastic Agents371372Concurrent use of antineoplastic agents may enhance the potential for renal 373toxicity, bronchospasm, and hypotension. Antineoplastic agents should be given concomitantly with caution.374375376Corticosteroids and Corticotropin (ACTH)377Concurrent use of corticosteroids and ACTH may potentiate hypokalemia which 378could predispose the patient to cardiac dysfunction. If used concomitantly, 379serum electrolytes and cardiac function should be closely monitored.380381Digitalis Glycosides382Concurrent use may induce hypokalemia and may potentiate digitalis toxicity.When administered concomitantly, serum potassium levels should be closely 383384monitored.385Flucytosine386387Concurrent use of flucytosine may increase the toxicity of flucytosine by 388possibly increasing its cellular uptake and/or impairing its renal excretion.389390Azoles (e.g. ketoconazole, miconazole, clotrimazole, fluconazole, etc.)391In vitro and in vivo animal studies of the combination of amphotericin B and 392imidazoles suggest that imidazoles may induce fungal resistance to 393amphotericin B. Combination therapy should be administered with caution, 394especially in immunocompromised patients.395396Leukocyte Transfusions397Acute pulmonary toxicity has been reported in patients simultaneously receiving 398intravenous amphotericin B and leukocyte transfusions.399400Other Nephrotoxic MedicationsConcurrent use of amphotericin B and other nephrotoxic medications may 401402enhance the potential for drug-induced renal toxicity. Intensive monitoring of 403renal function is recommended in patients requiring any combination of nephrotoxic medications.404405406Skeletal Muscle RelaxantsAmphotericin B-induced hypokalemia may enhance the curariform effect of 407408skeletal muscle relaxants (e.g. tubocurarine) due to hypokalemia. When 409administered concomitantly, serum potassium levels should be closely monitored.410411412Carcinogenesis, Mutagenesis, Impairment of Fertility413No long term studies in animals have been performed to evaluate carcinogenic414potential of Am B isome. Am B isome has not been tested to determine its 415mutagenic potential. A Segment I Reproductive Study in rats found an 416abnormal estrous cycle (prolonged diestrus) and decreased number of corpora 417lutea in the high dose groups (10 and 15 mg/kg, doses equivalent to human 418doses of 1.6 and 2.4 mg/kg based on body surface area considerations).419Am B isome did not affect fertility or days to copulation. There were no effects 420on male reproductive function.421422Pregnancy Category B423There have been no adequate and well-controlled studies of Am B isome in 424pregnant women. Systemic fungal infections have been successfully treated in 425pregnant women with amphotericin B deoxycholate, but the number of cases reported has been small.426427428Segment II studies in both rats and rabbits have concluded that Am B isome had no teratogenic potential in these species. In rats, the maternal non-toxic dose 429430of Am B isome was estimated to be 5 mg/kg (equivalent to 0.16 to 0.8 times the 431recommended human clinical dose range of 1 to 5 mg/kg) and in rabbits, 3 mg/kg (equivalent to 0.2 to 1 times the recommended human clinical dose 432433range), based on body surface area correction. Rabbits receiving the higher 434doses, (equivalent to 0.5 to 2 times the recommended human dose) of435Am B isome experienced a higher rate of spontaneous abortions than did the436control groups. Am B isome should only be used during pregnancy if the possible 437benefits to be derived outweigh the potential risks involved.438439Nursing Mothers440Many drugs are excreted in human milk. However, it is not known whetherAm B isome is excreted in human milk. Due to the potential for serious adverse 441442reactions in breast-fed infants, a decision should be made whether to 443discontinue nursing or whether to discontinue the drug, taking into account the importance of the drug to the mother.444445446Pediatric Use447Pediatric patients, age 1 month to 16 years, with presumed fungal infection 448(empirical therapy), confirmed systemic fungal infections or with visceral449leishmaniasis have been successfully treated with Am B isome. In studies whichincluded 302 pediatric patients administered Am B isome, there was no evidence 450451of any differences in efficacy or safety of Am B isome compared to adults. Since452pediatric patients have received Am B isome at doses comparable to those used in adults on a per kilogram body weight basis, no dosage adjustment is required 453454in this population. Safety and effectiveness in pediatric patients below the age455of one month have not been established. (See DESCRIPTION OF CLINICALSTUDIES -Empirical Therapy in Febrile Neutropenic Patients and 456457DOSAGE AND ADMINISTRATION.)。
注射用两性霉素B脂质体说明书【药品名称】通用名:注射用两性霉素B脂质体商品名:锋克松英文名:Amphotericin B Liposome(Ambisome)for Injection汉语拼音:Zhusheyong Liangxingmeisu B Zhizhiti本品主要成分为两性霉素B。
结构式:分子式:C47H73NO17分子量:924.09【性状】本品为淡黄色或黄色块状物【药理毒理】作用机理:两性霉素B脂质体的有效成分两性霉素B为多烯类抗真菌抗生素,它通过与真菌细胞膜上的固醇(主要为麦角固醇)结合,造成膜通透性改变,胞内容物流出而使真菌细胞死亡,两性霉素B也能结合哺乳动物细胞膜中的固醇(主要为胆固醇),这可能是其对动物和人类有毒性的原因。
本品是内含有两性霉素B的双层脂质体,其胆固醇成分可增强药物的稳定性,使两性霉素B尽可能在疏水层中保留最大的含量,降低与人体细胞膜中胆固醇的结合而增强对真菌细胞麦角固醇的结合,从而发挥两性霉素B的最大杀菌能力。
体外抗菌试验和临床试验提示:本品对新型隐球菌、白色念珠菌、热带念珠菌、酵母菌、总状毛霉、链互隔菌、曲霉菌、球孢子菌、组织胞浆菌、皮炎芽生菌、巴西芽生菌、孢子丝菌等有良好抗菌作用,但对细菌、立克次体、和病毒的感染无效。
皮肤和毛发癣菌大多耐药。
【药代动力学】本品未在中国人体内进行人体药代动力学研究。
动物药代试验中,本品静脉给药后,药物进入体内迅速分布至各组织,符合三室开放模型。
两性霉素B脂质体易被网状内皮系统的巨噬细胞所吞噬而较多地分布在肝、脾、肺,在各脏器内的浓度分布依次为肝、脾、肺、肾、心、脑、甲状腺,在各脏器的分布与普通两性霉素B不同,尤其在肾组织内浓度低,呈现非线性消除。
尚未进行转化和排泄研究。
【适应症】本品适用于诊断明确的敏感真菌所致的深部真菌感染,且病情呈进行性发展者,如败血症、心内膜炎、脑膜炎(隐球菌及其它真菌)、腹腔感染(包括与透析相关者)、肺部感染、尿路感染等。

分类号:R733.71学校代码:10392学科专业代码: 105101 学号:2101003217福建医科大学硕士研究生毕业论文卡泊芬净对比两性霉素B及其脂质体在治疗青少年及成人侵袭性真菌感染方面的meta分析Comparison of caspofungin and (liposomal) amphotericin B for treatment of invasive fungal infections in adolescents and adults : A meta-analysis学位类型:专业学位医学硕士所在学院:协和临床医学院研究张胜蓝生:学科、专业:内科学(血液)导沈建箴教授师:研究起止日期: 2012年9月至2013年5月答辩日期: 2013年06月06日二○一三年六月目录英汉缩略词对照 (4)中文摘要 (5)英文摘要 (6)前言 (8)目的 (12)方法 (12)结果 (14)讨论 (26)结论 (31)参考文献 (32)综述 (35)参考文献 (39)致谢 (42)英汉缩略词对照英文缩写英文全称中文全称IFI invasive fungal infection 侵袭性真菌感染CAS caspofungin 卡泊芬净AmB amphotericin B 两性霉素BLamB liposomal amphotericin B 脂质体两性霉素B RR relative risk 相对危险度CI confidence interval 置信区间RCT randomized controlled trial 随机对照临床试验ITT intension to treat 意向性治疗分析EBM evidence-based medicine 循证医学SR systematic review 系统评价卡泊芬净对比两性霉素B及其脂质体在治疗青少年及成人侵袭性真菌感染方面的meta分析摘要目的:随着广谱抗生素、免疫抑制剂、细胞毒药物的广泛应用及血液病、恶性肿瘤、免疫缺陷病等发病率的不断上升,侵袭性真菌感染的发病率也随之增加,因传统抗真菌药物疗效差、不良反应多导致病死率逐年上升。
两性霉素B脂质体的临床合理应用沈银忠【摘要】目的介绍临床如何合理使用两性霉素B脂质体(L-AmB).方法综述国内外文献,分析其药理特点、适应症和临床合理应用原则.结果两性霉素B(AMB)仍是治疗侵袭性真菌感染的主要药物,但众多的不良反应也限制了其在临床的广泛应用.L-AmB在保留AMB相似的抗真菌疗效的同时,减少了毒副作用.L-AmB具有抗真菌谱广、疗效稳定以及不易诱导真菌耐药等优点,可用于念珠菌病、曲霉、隐球菌病、马尔尼菲青霉病、组织胞浆菌病以及毛霉病等真菌病的治疗,尤其适于重症患者、孕妇以及因基础疾病而不适合使用或不能耐受AMB的患者以及对三唑类药物耐药的真菌感染和存在较多药物间相互作用的情况下,也可作为经验性抗真菌治疗的药物选择及高危人群侵袭性真菌感染的预防性用药.L-AmB价格较高,限制了其在临床的推广和使用.结论临床上应根据真菌感染的类型、感染部位、感染人群、基础疾病、肝肾功能状态、合并用药情况、不良反应、药物的可及性和可接受性等情况来合理使用L-AmB.有必要对L-AmB的临床应用价值和成本-效益进行进一步的研究.【期刊名称】《中国抗生素杂志》【年(卷),期】2015(040)007【总页数】5页(P495-499)【关键词】侵袭性真菌感染;两性霉素B脂质体;不良反应;适应症【作者】沈银忠【作者单位】上海市(复旦大学附属)公共卫生临床中心,上海201508【正文语种】中文【中图分类】R519;R978.5近年来,随着免疫缺陷人群尤其是艾滋病患者的增多,免疫抑制剂、广谱抗生素、肾上腺皮质激素的广泛使用,侵袭性真菌感染发病呈上升趋势,已经成为威胁人类健康的重要公共卫生问题,是患者就诊、入院和死亡的常见原因。
尽管新型抗真菌药物的出现为真菌感染提供了新的选择,但两性霉素B(amphotericin B,AMB)仍是目前治疗侵袭性真菌感染最基本和有效的抗真菌药物。
AMB抗真菌谱广,抗菌作用强,其疗效确切,但其不良反应尤其肾毒性较为突出,限制了其临床应用。
两性霉素B脂质体作为一线治疗药物:巴西内脏利什曼病卞星晨【期刊名称】《中国感染与化疗杂志》【年(卷),期】2018(018)004【总页数】1页(P364)【作者】卞星晨【作者单位】【正文语种】中文据估计,全世界每年约有2万至4万人死于内脏利什曼病(VL)。
VL是由利什曼原虫引起的人畜共患病,在巴西,每年大约有3 000例确证病例(2014年为3 453例),在大城市边缘的贫民窟流行,席卷整个国家。
巴西VL的发病率占拉丁美洲的95%以上。
世界卫生组织(WHO)推荐两性霉素B脂质体(LAMB)作为南美、地中海盆地、中东、中亚等地区治疗VL的一线治疗药物,其次为含锑制剂和两性霉素B脱氧胆酸盐(Ampho B)。
美国传染病协会/美国热带卫生学会指南也推荐LAMB作为该病的一线治疗药物。
但由于缺乏当地临床研究数据以及根据巴西当地专家意见,葡甲胺锑酸盐(MA)是一线用药,两性霉素B制剂仍作为二线用药,。
一项临床研究中,378例VL病患者(合并HIV感染者除外)随机分成4个治疗组:①Ampho B(1 mg·kg-1·d-1,疗程14 d);②LAMB(3 mg·kg- 1·d-1,疗程7 d);③MA(20 mg Sb5+·kg- 1·d-1,疗程20 d);④LAMB(单剂10mg/ kg)联合MA(20 mg Sb5+·kg-1·d-1,疗程20 d)。
Ampho B治疗组因毒性反应较多提前退出试验,其余3组共332例患者分析,结果发现治疗6个月后的治愈率MA为77.5%,LAMB为87.2%,LAMB联合MA为83.9%。
LAMB 与MA两组差异无统计学意义(P=0.222),但LAMB单药治疗的不良事件发生率、严重性以及导致治疗中止者(P=0.003)较MA治疗组具有更好的耐受性。
研究结果显示,LAMB是巴西和整个拉丁美洲VL病患者的首选治疗药物。

·综 述·注射用两性霉素B 脂质体临床药理学研究王曼曼1, 张雪媛1,2, 祁欢欢1, 尹佩华1, 肇丽梅2, 李春雷1关键词: 注射用两性霉素B 脂质体; 侵袭性真菌感染; 作用机制; 药动学; 有效性; 安全性中图分类号:R978.5 文献标识码:A 文章编号:1009-7708 ( 2021) 03-0362-07DOI: 10.16718/j.1009-7708.2021.03.022A review of clinical pharmacology of amphotericinB liposome for injectionWANG Manman, ZHANG Xueyuan, QI Huanhuan, YIN Peihua, ZHAO Limei, LI Chunlei [CSPC Zhongqi Pharmaceutical Technology (Shijiazhuang) Co., Ltd., Shijiazhuang 050035, China ]基金项目: 十三五“重大新药创制”国家科技重大专项(2018ZX0972*******)。
作者单位:1. 石药集团中奇制药技术(石家庄)有限公司,石家庄 050035;2. 中国医科大学附属盛京医院药学部。
第一作者简介: 王曼曼(1986—),女,硕士研究生,主要从事临床药理学研究。
通信作者:李春雷,E-mail :********************.com 。
1953年发现的两性霉素B 为多烯类抗真菌抗生素,是临床上治疗侵袭性真菌感染的“金标准”药物[1-2]。
两性霉素B 具有广泛的抗真菌谱,对念珠菌属、曲霉属都具有杀菌作用,抗真菌活性强,而且几乎没有耐药性[3]。
两性霉素B 去氧胆酸盐(amphotericin B deoxycholate, AmB-DOC )是首个用于临床的两性霉素B 普通制剂,临床应用已超过50年,也是应用最久的抗真菌药,但是其会产生不可逆的肾损伤、输液反应等严重的不良反应[2]。
北京雷根生物技术有限公司 两性霉素B 溶液(Amphotericin B,10mg/ml)简介:两性霉素B(Amphotericin B)是从Streptomyces nodosus 中分离出来的多烯类抗真菌(霉菌)的抗生素。
两性霉素B 作用原理在于其与真菌细胞膜上的Ergosterol 结合导致细胞膜通透性发生变化,使真菌细胞内钾离子、氨基酸通透到到膜外,破坏真菌正常代谢,进而使真菌细胞死亡。
由于细菌、病毒等细胞膜上并不含Ergosterol ,两性霉素B 对细菌、病毒并无抑制或杀灭作用,人和动物的细胞膜上含有与两性霉素 B 具有一定亲和力的胆固醇,所以其对人体会具一定毒性。
临床上,两性霉素B 主要用于治疗严重的以及深部的真菌感染。
Leagene Amphotericin B solution 主要用于生物科研领域,不用于临床。
组成:操作步骤(仅供参考):1、 根据实验具体要求操作。
注意事项:1、 注意无菌操作,避免污染。
2、 为了您的安全和健康,请穿实验服并戴一次性手套操作。
有效期:12个月有效。
相关:编号 名称 CA0040 Storage Amphotericin B solution(10mg/ml) 10ml 4℃ 避光 使用说明书 1份 编号 名称 CA0002 G418溶液(geneticin,20mg/ml) CA0075青霉素-链霉素混合溶液(100×双抗) CC0032Hanks 平衡盐溶液(1×HBSS,含酚红) DA0020Hoechst33342/PI 细胞凋亡染色试剂盒 DH0006苏木素伊红(HE)染色液 TC0713 葡萄糖检测试剂盒(GOD-POD 比色法)。
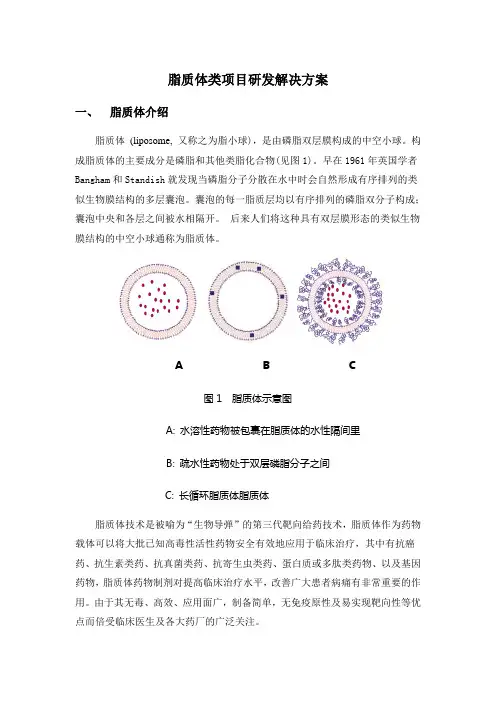
脂质体类项目研发解决方案一、脂质体介绍脂质体(liposome, 又称之为脂小球),是由磷脂双层膜构成的中空小球。
构成脂质体的主要成分是磷脂和其他类脂化合物(见图1)。
早在1961年英国学者Bangham和Standish就发现当磷脂分子分散在水中时会自然形成有序排列的类似生物膜结构的多层囊泡。
囊泡的每一脂质层均以有序排列的磷脂双分子构成;囊泡中央和各层之间被水相隔开。
后来人们将这种具有双层膜形态的类似生物膜结构的中空小球通称为脂质体。
A B C图1 脂质体示意图A: 水溶性药物被包裹在脂质体的水性隔间里B: 疏水性药物处于双层磷脂分子之间C: 长循环脂质体脂质体脂质体技术是被喻为“生物导弹”的第三代靶向给药技术,脂质体作为药物载体可以将大批已知高毒性活性药物安全有效地应用于临床治疗,其中有抗癌药、抗生素类药、抗真菌类药、抗寄生虫类药、蛋白质或多肽类药物、以及基因药物,脂质体药物制剂对提高临床治疗水平,改善广大患者病痛有非常重要的作用。
由于其无毒、高效、应用面广,制备简单,无免疫原性及易实现靶向性等优点而倍受临床医生及各大药厂的广泛关注。
目前已生产上市的脂质体药物多属常规脂质体和长效脂质体。
常规脂质体利用磷脂组成的双层膜将药物包裹在脂质体囊泡中。
其主要功能为降低药物毒性和增强药效,比如:脂质体两性霉素 (商品名,AmBisome),脂质体阿霉素 (Myocet) 和脂质体柔红霉素 (DaunoXome)。
而长效脂质体是表面用聚乙二醇-磷脂衍生物(PEG-lipids)修饰了的脂质体。
修饰后的脂质体提高了药物在血液中的保留时间,增加了药物的被动靶向功能。
聚乙二醇-脂质体阿霉素(Doxil) 已经在欧美生产上市。
二、项目案例及技术方案虽然脂质体的制备可以细分为薄膜分散法、逆相蒸发法、有机溶剂注入法等许多种,但从所要装载的药物性质的不同以及脂质体药物制剂大规模工业生产的角度主要以pH梯度法及薄膜分散法两种,下面将以两个典型案例展示。

氨磷汀 (Amphotericin B) 抗真菌药物氨磷汀 (Amphotericin B) 抗真菌药物氨磷汀(Amphotericin B)是一种广谱抗真菌药物,常用于治疗严重的真菌感染疾病。
它具有独特的机制,能够杀灭或抑制多种真菌的生长,包括寄生真菌和霉菌等病原体。
氨磷汀的药效和不良反应非常值得关注,本文将介绍氨磷汀的药理作用、临床应用、使用方法、不良反应以及注意事项。
一、药理作用氨磷汀是一种聚醚类抗真菌药物,通过与真菌细胞膜中的麦角固醇结合,改变细胞膜的通透性,从而破坏真菌细胞壁和细胞膜,引起真菌细胞的死亡。
传统的氨磷汀是非选择性麦角固醇结合剂,也可与人体细胞膜中的胆固醇结合,但现代氨磷汀的结构改良使其选择性结合真菌细胞膜中的麦角固醇而不结合胆固醇,从而减少对人体细胞的不良影响。
二、临床应用氨磷汀主要用于治疗严重的真菌感染疾病,如念珠菌病、组织胞浆菌病和曲霉病等。
它广谱杀菌,对于各种感染都有很好的疗效,尤其在对多种真菌耐药的情况下仍然有效。
在临床上,氨磷汀通常用于重症真菌感染的治疗,例如血流感染和器官浸润等情况。
此外,氨磷汀还可以用于预防高危人群的真菌感染,如血液恶性肿瘤患者和器官移植后的患者等。
三、使用方法氨磷汀的给药途径包括静脉注射和局部涂抹。
由于氨磷汀具有强烈的肾毒性,静脉注射时需要非常谨慎。
一般情况下,氨磷汀的剂量根据患者的体重和肾功能来确定,通常每日剂量为0.3-1.5毫克/千克体重。
治疗期间需要监测患者的肾功能和血液学指标,如肌酐清除率和血小板计数等。
四、不良反应氨磷汀的不良反应主要包括肾毒性、静脉注射反应和电解质紊乱等。
肾毒性是最为严重的副作用,可导致肾功能损害和肾衰竭。
静脉注射时,常见的不良反应有寒战、发热、头痛、恶心和呕吐等。
而电解质紊乱主要表现为低钾血症、低镁血症和低钙血症等。
在使用氨磷汀期间,应定期监测患者的肾功能和电解质水平。
五、注意事项在使用氨磷汀时,需要特别注意以下几点。
某院重症监护室特殊使用级抗生素应用分析【摘要】目的:分析某医院重症监护室患者特殊级抗菌药物的用药情况,为规范临床合理用药提供参考。
方法:抽取 2020 年1 月—2020 年 12 月间ICU住院患者特殊使用级抗菌药物用药医嘱,统计和分析其各特殊级抗菌药物的用药频度(DDDs)、联合用药、不合理用药情况。
结果:ICU住院患者特殊级抗菌药物 DDDs 最高的是美罗培南(1015.83),其次是比尔培南(277.5),最低的是两性霉素b脂质体(6.29);联合用药以一联为主,共使用168例次,一联药物中美罗培南使用频率最高;其次是二联用药,共使用111例次,二联以美罗培南联合去甲万古霉素使用频率最高。
一联和二联总占比为92.69%。
结论:医院特殊使用级抗菌药物的使用主要以一联和二联为主。
使用情况基本合理,但仍需严格掌握抗菌药物使用指征,严格管理确保住院患者临床用药的安全性和合理性。
关键词:抗菌药物;用药频度;联合用药重症监护室是运用先进医疗设备和临床监测技术对患者进行有力治疗照护及精细病情监测的部门[[1]]。
ICU患者特点不仅疾病重,而且往往伴随严重的基础疾病,抵抗力差,嵌入性操作多等特点,导致患者继发感染的几率大大增加。
而长期不合理使用抗生素容易导致泛耐药菌感染发生已成为大部分学者的共识。
特殊使用级抗菌药物及时正确的使用对ICU患者的救治起到非常重要的作用。
特殊使用级抗菌药物指: ①有显著或比较严重的副作用,不适合随意应用; ②具备极强的抑菌作用、抗菌谱广。
经常或过多应用会造成病原菌过快地产生耐药性; ③疗效和安全性数据信息较少,不优于现阶段应用的药物; ④新上市的抗菌药物,在适应症,疗效或安全性方面尚需进一步考证的、价格昂贵的抗菌药物[[2]]。
特殊使用级抗菌药物要求医师必须经具有相应处方权限, 并经具有抗感染临床经验的感染或相关专业专家会诊同意后, 方可使用[[3]]。
本文综合分析某院ICU 2020 年1月~2020 年12月特殊使用级抗菌药物(以下简称特抗药)使用情况,主要包括药品用量、联合用药、不合理用药等信息,为临床合理使用及科学管理特抗药提供参考。
国家药品监督管理局通告2020年第30号——国家药监局关于发布仿制药参比制剂目录(第二十七批)的
通告
文章属性
•【制定机关】国家药品监督管理局
•【公布日期】2020.04.29
•【文号】国家药品监督管理局通告2020年第30号
•【施行日期】2020.04.29
•【效力等级】部门规范性文件
•【时效性】现行有效
•【主题分类】药政管理
正文
国家药品监督管理局通告
2020年第30号
国家药监局关于发布仿制药参比制剂目录(第二十七批)的
通告
经国家药品监督管理局仿制药质量与疗效一致性评价专家委员会审核确定,现发布仿制药参比制剂目录(第二十七批)。
特此通告。
附件:仿制药参比制剂目录(第二十七批)
国家药监局
2020年4月29日附件
仿制药参比制剂目录(第二十七批)。
两性霉素B脂质体治疗血液病患者侵袭性真菌感染2例并文献复习摘要目的:探讨两性霉素B脂质体在血液病患者侵袭性真菌感染的应用时机、疗效及如何减少不良反应。
方法:回顾我院2例应用两性霉素B脂质体成功治疗血液病晚期患者侵袭性真菌感染的治疗过程。
结果:1例为老年白血病患者,化疗后粒细胞缺乏期应用三唑类药物预防真菌感染失败,出现真菌败血症,改用两性霉素B抢先治疗后获得痊愈;另1例为原发性骨髓纤维化晚期患者,长期粒细胞缺乏导致颅内侵袭性真菌感染,应用三唑类药物治疗无效,及时更换两性霉素B脂质体后取得良好疗效。
结论:两性霉素脂质体B具有很好的组织渗透性,治疗侵袭性真菌感染患者能降低病死率,能透过血脑屏障有效治疗颅内侵袭性真菌感染;脂质体剂型能有效降低两性霉素B的毒副作用。
ABSTRACT Objective:To investigate the indications,efficacy and toxicity of liposomal amphotericin B in the treatment of invasive fungal infection in patients with hematological diseases. Methods:Two hematological patients with invasive fungal infection were successfully treated and their cases were retrospectively analyzed. Results:An elderly patient with leukemia failed to be treated with triazole antifungal agents as prophylaxis therapy after developed neutropenia following chemotherapy and he was diagnosed as fungal septicemia,then was treated with amphotericin B as a preemptive therapy and got a full recovery. Another patient with late stage primary myelofibrosis suffered from intracranial invasive fungal infection due to long term of neutropenia. He was treated with amphotericin B and obtained a good therapeutic effect after failed to be treated with triazole antifungal agents. Conclusion:Liposomal amphotericin B has a good tissue penetrative ability,can reduce mortality when applied in the treatment of patients with invasive fungal infection,and can pass through the blood-brain barrier resulting in effective treatment of intracranial fungal infection. Its liposome formulation can effectively reduce the adverse effects related to amphotericin B.KEY WORDS liposomal amphotericin B;invasive fungal infection;intracranial infection;fungal septicemia粒细胞缺乏的血液病患者容易合并侵袭性真菌感染,严重时可致真菌败血症或重要脏器感染。
ADME Studies in Support of Development of Liposomal Formulations of MarketedChemotherapeuticsDennis Heller,Ph.D.XenoBiotic Laboratories,Inc.Presentation Outline∙Review of Liposomal Drug Delivery∙Regulatory Requirements for ADME/PK Data ∙Case Study:CPX-351∙Introduction to CPX-351Development∙Non-clinical ADME Study Results∙SummaryLiposomal Drug DeliveryLiposomes–General Properties•A liposome is an artificially-prepared spherical vesicle composed of a lipid bilayer.•Liposomes are often composed of phosphatidylcholine-enriched phospholipids and may also contain mixed lipid chains with surfactant properties such as egg phosphatidylethanolamine.The major types of liposomes are the multilamellar vesicle(MLV),the small unilamellar vesicle(SUV),the large unilamellar vesicle(LUV),and the cochleate vesicle.•A liposome encapsulates a region of aqueous solution inside a hydrophobic membrane;dissolved hydrophilic solutes cannot readily pass through the lipids.Hydrophobic chemicals can be dissolved into the membrane,and in this way liposome can carry both hydrophobic molecules and hydrophilic molecules.•To deliver the molecules to sites of action,the lipid bilayer can fuse with other bilayers such as the cell membrane,thus delivering the liposome contents.By making liposomes in a solution of DNA or drugs(which would normally be unable to diffuse through the membrane) they can be(indiscriminately)delivered past the lipid bilayer.Liposomal Drug DeliveryBy encapsulating a drug(s)in a liposome,the PK/PD profile may be improved compared to the non-liposomal form.Liposomal drug delivery systems may be designed to shape the drug disposition profile to:–increase the circulation time within the body(e.g.via protective PEGylation)avoiding detection“steath”,thus increasing theexposure profile to disease cells/tissues,–target(active(peptide or mab)or passive)and release within specific disease tissue types,and–minimize the harmful effects on healthy tissues(e.g.cardio or liver toxicity).Pharmacokinetics of Radioactivity in PlasmaList of Clinically Approved Liposomal Drugs as of2012Name Trade name Company Indication Liposomal ExcipientsLiposomal amphotericin B Abelcet Enzon Fungal infections DMPC,DMPGLiposomal amphotericin B Ambisome Gilead Sciences Fungal and protozoalinfectionsHSPC,Cholesterol,DSPGLiposomal cytarabine Depocyt Pacira(formerlySkyePharma)Malignant lymphomatousmeningitisDOPC,Cholesterol,DPPGLiposomal daunorubicin DaunoXome Gilead HIV-related Kaposi’ssarcomaDSPC,CholesterolLiposomal doxorubicin Myocet Zeneus Combination therapy withcyclophosphamide inmetastatic breast cancerLIPOVA-E120,CholesterolLiposomal IRIV vaccine Epaxal Crucell Hepatitis A LECIVA-S70Liposomal IRIV vaccine Inflexal V Berna Biotech Influenza LECIVA-S90Liposomal morphine DepoDur SkyePharma,Endo Postsurgical analgesia DOPC,Cholesterol,DPPG Liposomal verteporfin Visudyne QLT,Novartis Age-related maculardegeneration pathologicmyopia ocularhistoplasmosisEgg PG,DMPCLiposome-proteins SP-B and SP-C Curosurf Chiesi Farmaceutici,S.p.A.pulmonary surfactant forRespiratory DistressSyndrome(RDS)Leciva-S90Liposome-PEG doxorubicin Doxil/Caelyx Ortho Biotech,Merck HIV-related Kaposi’ssarcoma,metastatic breastcancer,metastatic ovariancancerMPEG-DSPE,HSPC,CholesterolLiposomal vincristine Marqibo Spectrum Pharmaceuticals Acute LymphoblasticLeukemia(ALL)andMelanoma Cholesterol and egg sphingomyelinLipid Soluble Drug in the BilayerHydrophilic Drug Contained within the LiposomeLiposomal Drug Development Regulatory Requirements for ADME/PK DataFDA Draft-Guidance for Industry(Aug,2002) Liposomal Drug Products–CMC;Human Pharmacokinetics and Bioavailability;Labeling and DocumentationIntroduction…“A drug substance in a liposome formulation is intended to exhibit a different pharmacokinetic and/or tissue distribution(PK/TD)profile from the same drug substance(or active moiety)in a nonliposomal formulation given by the same route of administration.The complete characterization of the PK/TD profile of a new liposome drug product is essential to establish the safe and effective dosing regimen of the product”…This guidance does not cover clinical efficacy and safety studies or bioequivalence studies of those to document sameness./downloads/Drugs/GuidanceComplianceRegulatoryInformation /Guidances/ucm070570.pdfA.Bioanalytical Methods…for liposomal drug products the bioanalytical method should alsobe capable of measuring encapsulated and unencapsulated drug substance.B.In Vivo Integrity(Stability)Considerations…if the bioanalytical method can distinguishbetween encapsulated and unencapsulated drug substance,the in vivo stability of the liposome should be determined.The liposome is considered stable in vivo,if over time(from PK study),the:•Drug substance,when in circulation,remains substantially in the encapsulated form.•Ratio of unencapsulated to encapsulated drug substance remains constantWhen the liposome is stable in vivo,the total drug substance can be measured todetermine the PK and Bioavailability.C.Protein BindingD.In Vitro StabilityFDA Draft Guidance–Liposomal Drug Products,2002E.Pharmacokinetics and Bioavailability•ADME/PK parameters may be different between the liposome and nonliposome drug products.•Conduct comparative MB/PK studies between the liposome and nonliposome drug products when(1)the two products have the same active moiety,(2)the two products are given by the same route of administration,and(3)one of the products is already approved for marketing.1.Mass Balance(MB)Study•a crossover or non-crossover design•drug substance tagged with a radioactive label(e.g.14C,3H)2.PK Studies•Single Dose,Multi-dose,dose proportionality(measure encapsulated and unencapsulated drug substance if needed)3.Additional PK Studies•Food-Effect•Drug Interaction and/or Special Populations•Exposure-responseFDA Draft Guidance–Liposomal Drug Products,2002EMA(European Medicines Agency)CHMP(Committee for Human Medicinal Products)–21Feb2013Reflection paper on the data requirements for intravenous liposomal products developed with reference to an innovator liposomal productIntroduction“…liposomal medicinal products have formulation and manufacturing-specific distribution characteristics after intravenous administration and similar plasma concentrations may not correlate with therapeutic performance…the complete characterisation of the stability,pharmacokinetics(including tissue distribution) of a new liposomal product is critical to establish safe and effective use.This is because differences between the applicant’s product and innovator product with regard to manufacturing process steps and formulation may substantially modify efficacy/safety due to changes in specific liposome-cell interactions and liposome distribution characteristics which are not detectable by conventional bioequivalence testing alone”.http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/ 2013/03/WC500140351.pdf3.2Non-Clinical and Clinical Requirements✓Significant changes in pharmacokinetic characteristics are evident when an active substance is administered in a liposomal formulation,i.e.volume of distribution and clearance may be reduced and half-life prolonged.The clearance of the liposomal active substance isdependent on:1.the clearance of the liposomal carrier itself,2.the rate of release of entrapped drug from the liposomal carrier,and3.the clearance and metabolism of unencapsulated drug upon its release.✓The rate and location of in vivo drug release is a crucial parameter which can affect toxicity and efficacy.✓Therefore,the pharmacokinetics of the developed liposomal product should always be compared with the innovator’s product.Only certain aspects of the conventionalbioequivalence approach are applicable and in some cases additional requirements should be set on a case-by-case basis.✓Comparative human pharmacokinetic investigations should demonstrate not only the similarity of exposure of the total,unencapsulated and liposome encapsulated drug,but they should also demonstrate similar distribution and elimination characteristics.EMA Reflection Paper–20133.2.3Non-clinical Studies(ADME requirements!)Non-clinical pharmacokinetic studies•Some pharmacokinetic aspects of liposomal products with regard to their performance in humans can be predicted by animal and,where applicable,cell-based models.However,the choice of appropriate species and models to investigate the in-vivo release of the drug from liposomes should be justified with special emphasis on areas such as accumulation and retention in target organs,pharmacokinetics and distribution.In addition to the systemic exposure,similarities in the distribution and elimination should be demonstrated.These studies provide pivotal evidence of the comparability of disposition of liposomal drug products,as it is not possible to have a full picture of the distribution in man from blood/plasma data alone.•time points and sampling duration should be carefully selected so as to accurately Samplingquantify the time course of unencapsulated and total drug and metabolite in tissuesbalancing the need to quantify early drug release from liposomes(e.g.over first15min)and persistence of drug in particular tissues.If due to analytical reasons free concentrations cannot be measured then attempts should be made to compare the metaboliteconcentrations in the target organs.•Analytes to be measured–The kinetics(including tissue distribution and excretion)of both the unencapsulated drug and the encapsulated drug should be investigated if feasible.EMA Reflection Paper–2013Combination ChemotherapyFor most patients with cancer,standard of care usually involves the use of combinations of individual drugs. For example,the use of cytarabine in combination with an anthracycline(such as daunorubicin)is the standard of care for the treatment of patients diagnosed with acute myeloid leukemia(AML).Individual drugs are combined at their“maximum tolerated dose”(MTD),the dose at which a drug has been shown to deliver maximum benefit balanced by an acceptable level of toxicity.Complementary mechanism of actionsUnderstanding the Impact of Drug Ratios Dosing individual drugs at MTD does not always produce combination drug regimens that deliver maximum efficacy.The same drugs combined at different ratios can result in distinctly varied efficacy and safety profiles.Depending on the ratio of the combined drugs,the outcome can be:Additive–the anti-cancer effect of the drugs is equal to the sum of the individual drugs.Synergistic–the anti-cancer effect of the drugs is greater than the sum of the individual drugs.Antagonistic–the anti-cancer effect of the drugs is less than the sum of the individual drugs.SummaryNon-clinical ADME Studies to support Liposomal Drug Development•Comparative studies of free vs.encapsulated forms of radiolabel drug(s)provide key information required by agencies for approval.•May help to reduced the number and scope of additional clinical trials required for regulatory approval.Thank you。
卡泊芬净与脂质体两性霉素B在血液病患者经验性抗真菌治疗中的比较【摘要】目的评价和比较卡泊芬净与脂质体两性霉素B在血液病患者经验性抗真菌治疗的有效性和安全性。
方法采取随机、对照、开放的临床试验研究,选取出现不明原因发热、广谱抗生素治疗3~7d无效且被真菌感染的高危因素血液病患者。
将60例入选患者随机分为两组,卡泊芬净组(32例)静脉滴注卡泊芬净(d1 70mg,d2起50mg/d);脂质体两性霉素B组(28例)静脉滴注脂质体两性霉素B [3mg/(kg・d)]。
两组治疗时间持续至中性粒细胞恢复和症状消失后5d,或者疗程大于10d。
观察两组患者的疗效和不良反应。
结果共有60例患者接受评估,卡泊芬净组32例,总有效率65.6%,不良反应率25.0%;脂质体两性霉素B组28例,总有效率67.9%,不良反应率71.4%。
两组总有效率无显著性差异,但卡泊芬净组不良反应率显著低于脂质体两性霉素B组。
结论对血液病患者的经验性抗真菌治疗,卡泊芬净的疗效与脂质体两性霉素B相当,但耐受性较脂质体两性霉素B 好。
【关键词】卡泊芬净两性霉素B 脂质体真菌感染Comparison of caspofungin and liposomal amphotericin B forempirical antifungal therapy in patients with hematologic diseaseABSTRACT Objective To compare the efficacy and safety of caspofungin with liposomal amphotericin B for empirical antifungal therapy of fungal infection in patients with hematologic diseases. Methods Sixty cases of patients with high risk factors of systemic fungal infections and unexplained fever that did not respond tobroad��spectrum antibiotic therapy for 3~7 days were randomly pided into 2 groups. Caspofungin group (32 cases) were administered with caspofungin intravenously 70 mg on day 1 and 50 mg once daily thereafter compared with patients in the other group (28 cases) receiving liposomal amphotericin B, 3 mg/(kg·d). Both of the treatments were conti nued until five days after neutropenia and fever had resolved or the drug had been administered for at least 10 days. Adverse events and the efficacy were investigated. Results For caspofungin group (n=32) and liposomal amphotercin B group the overall effective rates were 65.6% and 67.9%,and the adverse reactions rates were 25.0% and 71.4%, respectively. There were no significant differences in the overall effective rates between two groups, but the adverse reactions occurrence of caspofungingroup was lower than liposomal amphotericin B group. Conclusions Caspofungin is as effective as liposomal amphotericin B and with fewer ADRs in the treatment of fungal infection in patients with hematologic diseases.KEY WORDS Caspofungin; Amphotericin B; Liposomes; Fungal infection近年来,临床观察显示侵袭性真菌感染的比例有逐渐增高的趋势,已成为造血干细胞移植、脏器移植以及其他免疫缺陷患者治疗过程中最主要的障碍之一。
传统两性霉素B和脂质体两性霉素B治疗血液病患者安全性的回顾性队列研究徐芳菲;梁密;黄伟【期刊名称】《中国真菌学杂志》【年(卷),期】2024(19)1【摘要】目的比较传统两性霉素B(conventional amphotericin B,C-AMB)和脂质体两性霉素B(liposomal amphotericin B,L-AMB)治疗血液病患者的安全性。
方法收集2016年—2022年于华中科技大学同济医学院附属同济医院血液科接受C-AMB或L-AMB治疗的血液病患者信息,通过倾向性匹配评分分析法将两组患者年龄和性别进行匹配后,比较两组患者治疗过程中出现的药物不良反应。
结果两组患者在治疗总时间,因治疗成功或失败而停药的发生率,因低钾血症、肝毒性和肾毒性等不良反应导致停药的发生率均无明显差异。
两组患者在肾毒性和低钾血症发生率方面也没有明显差异。
但是,两性霉素B的单日最大剂量是影响其相关肾毒性和低钾血症的关键因素。
结论C-AMB仍然是一种值得在临床中使用的安全有效的药物,特别是对于经济条件较差、需要接受经验性或抢先抗真菌治疗的血液病患者。
【总页数】7页(P8-14)【作者】徐芳菲;梁密;黄伟【作者单位】华中科技大学同济医学院附属同济医院血液科;北京大学人民医院血液科【正文语种】中文【中图分类】R978.5【相关文献】1.两性霉素B脂质体治疗血液病患者侵袭性真菌感染2例并文献复习2.卡泊芬净与脂质体两性霉素B在血液病患者经验性抗真菌治疗中的比较3.国产两性霉素B 抢先治疗血液病患者肺部侵袭性真菌感染的疗效与安全性分析4.卡泊芬净与两性霉素B脂质体对儿童血液病患者伴真菌感染的临床疗效与安全性对照研究因版权原因,仅展示原文概要,查看原文内容请购买。
Liposomal amphotericin B(AmBisomeÒ)efficacy in confirmed invasive aspergillosis and otherfilamentous fungal infections in immunocompromised hosts:a pooled analysisC.Cordonnier,1M.Bresnik2and R.Ebrahimi21Service d’He´matologie Clinique,Hoˆpital Henri Mondor,Creteil,France and2Gilead Sciences,Foster City,CA,USASummary A pooled efficacy analysis applying current diagnostic standards for case selection wasperformed on previously published trials of liposomal amphotericin B for invasivefilamentous fungal infections(IFFI).Favourable responses were observed in51%ofmicrobiologically confirmed cases of proven or probable IFFI.Despite the limitationsinherent in a retrospective analysis of pooled studies,the response rates observed in thisanalysis were consistent with previous reports for antifungal therapy withamphotericin B deoxycholate or voriconazole in the treatment of invasive aspergillosis. Key words:AmBisome,amphotericin B,aspergillosis.IntroductionInvasive aspergillosis(IA)and other invasivefilamen-tous fungal infections(IFFI)continue to be associated with significant morbidity and mortality,particularly in immunocompromised patients.Efficacy and survival rates for antifungal therapies for the treatment of IFFI have varied considerably depending on the patient population studied[e.g.underlying disease,allogeneic stem cell transplantation(SCT),presence and severity of neutropenia,and receipt of immunosuppressive therap-ies].The liposomal formulation of amphotericin B(L-AMB)exhibits a broad spectrum of activity against yeast and moulds comparable with amphotericin B deoxych-olate1but with a more favourable safety profile that significantly reduces dose-limiting toxicities associated with amphotericin B deoxycholate.2,3The efficacy and safety of L-AMB have been reported in a number of randomised comparative trials,3,4as well as in open-label trials and retrospective analyses.5–9Subsequent to the publication of these studies,diagnostic criteria for defining and classifying proven and probable cases of IFFI in immunocompromised patients for inclusion in antifungal efficacy trials have been made uniform.10To further define the efficacy of L-AMB in the treatment of IA and other IFFI for patients treated in clinical trials before2002,a pooled analysis of four prospective, clinical trials was performed,applying the currently accepted diagnostic standards for case selection and efficacy analyses.Materials and methodsPatient populationOriginal case report forms(CRF)for patients treated with1–15mg kg)1day)1L-AMB[AmBisome;Gilead Sciences,Inc.,Foster City,CA(formerly Nexstar)and Fujisawa Healthcare,Inc.,Deerfield,IL,USA]collected from four clinical studies were reviewed individually. The CRF were obtained from three published,prospect-ive,multicentre clinical trials.3–5These studies included: L-AMB5mg kg)1day)1vs.amphotericin B deoxycho-late for the treatment of documented and suspected neutropenia-associated invasive fungal infections,3 L-AMB1mg kg)1day)1vs.L-AMB4mg kg)1day)1 for the treatment of IA4and a safety,tolerance and pharmacokinetic trial of high-dose L-AMB(7.5–15mg kg)1day)1).5The fourth study was a compas-sionate-use,multicentre study,from which cases have been previously reported in four publications.6–9Correspondence:Catherine Cordonnier,Service d’He´matologie Clinique,Hoˆpital Henri Mondor,51Avenue du Marechal de Lattre de Tassigny,CreteilCedex94010,France.Tel.:+33(0)149812059.Fax:+33(0)149812067.E-mail:carlcord@club-internet.frAccepted for publication27December2006Original articleJournal CompilationÓ2007Blackwell Publishing Ltd•Mycoses(2007),50,205–209Methodology and analysisThe diagnosis of proven or probable IFFI was deter-mined using criteria defined by the European Organisa-tion for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group(EORTC/MSG).10Cases were confirmed by histopathology or were microbiologically confirmed by culture or Aspergillus antigen.This was required so as to increase the level of certainty of IFFI and to avoid the inclusion of misleading cases only documented through imaging(e.g.halo sign or air-crescent sign).Chest computerised tomography scan abnormalities were assumed to be non-halo infiltrates(i.e.minor EORTC/ MSG criterion)unless otherwise stated.Additional clinical signs and symptoms of infections reported in the CRF were required to fulfil clinical criterion for IFFI. All cases with the protocol-defined IFFI that met EORTC/MSG criteria for proven or probable IFFI and in which greater than or equal to one dose of L-AMB was administered were included in the pooled analysis.A favourable response(plete or partial response) was based on the investigator-determined assessments, in which criteria for complete and partial responses were previously defined per each protocol.3–9Death or discontinuation from the study before response assess-ment could be made was considered a failure of therapy for this analysis.Survival was determined from the last follow-up visit reported in the CRF.ResultsPatientsA total of212cases were screened,of which69(33%) cases met the EORTC/MSG criteria for proven(n¼20) or probable(n¼49)IFFI.The proven and probable cases were identified infive of26cases reported in Leenders et al.[3],25of115cases reported in Ellis et al.[4],21of44cases reported in Walsh et al.[5]and18of 27cases reported in the compassionate-use trial.6–9 Rejected cases included137cases that lacked a micro-biologically documented fungal pathogen and six cases that lacked appropriate host factors,including malig-nancy,organ transplant or infection with human immunodeficiency virus.Of the69confirmed proven or probable cases,microbiologic data used to confirm the diagnosis of IFFI included positive culture(n¼59), positive Aspergillus antigen assay(n¼3)and histopa-thology(n¼13).Six cases had both a positive culture and documented histopathology.The most common fungal isolate identified was Aspergillus species(n¼61), with six Zygomycetes and four Fusarium isolates were also documented.The majority of patients(n¼61;88%)had haema-tological diseases,with38patients diagnosed with acute leukaemia.Of these61patients,30%(n¼18) had received an allogeneic SCT.Eight of the69patients had undergone a solid organ transplant,had a solid tumour or were infected with human immunodeficiency virus.There were51(74%)males included in the analysis,and the median age of the patient population was43years(range,14–72years).The median L-AMB dose administered was4mg kg)1day)1(range,1–15mg kg)1day)1),with48cases treated with L-AMB 1–5mg kg)1day)1and21cases treated with L-AMB 7.5–15mg kg)1day)1.L-AMB was administered as thefirst-line therapy in44patients and as the second-line therapy in25patients(20because of failure of the first-line treatment andfive because of amphotericin B-induced nephrotoxicity).None of the patients treated with L-AMB as the second-line therapy had received voriconazole or an echinocandin before entry into the trials.ResponseA favourable response(complete response,n¼15; partial response,n¼20)with L-AMB was observed in 35of69(51%)cases:11of20(55%)cases of proven IFFI and24of49(49%)cases of probable IFFI(Table1). Treatment with L-AMB as thefirst-line therapy showed a higher favourable response(61%)compared with the administration of the second-line therapy(32%).In addition,patients with severe neutropenia(absolute neutrophil count<500cells mm)3)at baseline showed a response similar to that of patients without severe neutropenia,with16of34(47%)patients and19of35 (54%)patients achieving a favourable response respect-ively(Table1).In patients with haematological disease, a favourable response was observed in31of61(51%) patients(Table1).Of these61patients,eight of18 (44%)who received allogeneic SCT and four of seven (57%)who received autologous SCT showed a favour-able response with L-AMB.Favourable response rates varied by the site of infection,ranging from44%(21of48cases)for pulmonary infections,64%(seven of11cases)for sinus/nasal infections,57%(four of seven cases)for disseminated infections and one of one case each for subcutaneous abscess,pericarditis,and mastoiditis (Table1).Favourable response rates by pathogen indi-cated that L-AMB was effective against Aspergillus,C.Cordonnier et al.Journal CompilationÓ2007Blackwell Publishing Ltd•Mycoses(2007),50,205–209Zygomycetes and Fusarium pathogens.A favourable response was observed in28of59(47%)patients with IA,five of six(83%)patients with zygomycosis and two of four patients with fusariosis.There were no apparent trends in response rates based upon the dose of L-AMB received(Table2).SurvivalOf the69patients with probable or proven IFFI,35 (51%)patients treated with L-AMB survived to the last follow-up visit.Three of the patients who survived were from the clinical trial reported by Leenders et al.[3],15 patients were from Ellis et al.[4],nine patients were from Walsh et al.[5],and eight patients were from the compassionate-use trial.6–9Of these surviving patients, 23of35patients had survival documented to ‡12weeks after the initiation of treatment.For the remaining12patients whose last study visit was <12weeks following the initiation of L-AMB treatment, the mean follow-up time was65days(range,31–82days).DiscussionThe consensus guidelines defining the criteria for the diagnosis of invasive fungal infections10were developed to standardise the inclusion of patients in clinical trials. Cases of IFFI reported from studies before the latest standardisation of the diagnostic criteria by EORTC/ MSG are difficult to assess because of the inclusion of ÔsuspectedÕorÔprobableÕcases that lacked microbiologic confirmation of a fungal pathogen.Many of these cases were presumed to be aspergillosis based on fevers unresponsive to broad-spectrum antibacterial therapy, new and/or persisting pulmonary infiltrates and lack of isolation of specific pathogens.These would be charac-terised as possible cases by the current EORTC/MSG definitions.Furthermore,this has made it difficult to compare more recently conducted antifungal clinical studies to historic controls.Applying these newer diagnostic standards for identifying proven or probable IFFI to previously reported cases treated with L-AMB demonstrated a favourable response rate(complete or partial response)of51%in a population of69severely immunocompromised patients with microbiologically confirmed IFFI.Because of the small number of patients treated at each dose level(1–15mg kg)1day)1)and the different protocols followed,we cannot draw any conclusions on the dose-related efficacy of L-AMB in proven or probable infections.However,these data help reaffirm the efficacy of L-AMB,using currently accepted standards for documenting IFFI.Additionally,these response rates are consistent with the results that were recently reported in a prospective,randomised trial of two dose regimens of L-AMB(3mg kg)1day)1vs. 10mg kg)1day)1)in confirmed mould infections(Am-BiLoad trial).In this study,favourable response rates were found in50%and46%of patients in the standard-and high-dose groups respectively.11Applying these newer diagnostic standards also allowed for more precise determination of IA cases and for consideration of the efficacy results in the context of prospective studies recently reported.12,13Table1Response rates according to presentation,treatmentindication,underlying disease and site of infection.Overall response,n/n(%)1Total352/69(51;95%CI39–63)Diagnosis categoryProven11/20(55)Probable24/49(49)Treatment indicationFirst-line therapy27/44(61)Second-line therapy8/25(32)After failure offirst-line treatment6/20(30)Because of nephrotoxicity2/5(40)Neutropenia at baselineANC<500cells mm)316/34(47)ANC‡500cells mm)319/35(54)Status of underlying haematological disease3Uncontrolled419/40(48)Controlled412/21(57)Underlying diseaseHaematological disease31/61(51)Acute leukaemia25/38(66)Chronic myeloproliferative disorders1/4(25)Lymphoproliferative disorders3/8(38)Aplastic anaemia1/5(20)Myeloma1/6(17)Allogeneic stem cell transplantation8/18(44)Solid organ transplant0/3(0)Solid tumour2/2(100)HIV infection2/3(67)SitePulmonary21/48(44)Sinus/nasal7/11(64)Disseminated4/7(57)Other53/3(100)ANC,absolute neutrophil count;HIV,human immunodeficiencyvirus.1Complete or partial response.2Complete response¼15;partial response¼20.3Eight patients had non-haematological conditions.4Uncontrolled disease¼evidence of active disease present at studyentry.5One site each of subcutaneous abscess,pericardium or mastoidprocess.Liposomal amphotericin B efficacy Journal CompilationÓ2007Blackwell Publishing Ltd•Mycoses(2007),50,205–209In an open-label,non-comparative trial of116patients with acute IA,13a complete or partial response was reported in35of60(58%)patients treated with voriconazole as afirst-line therapy and21of56 (38%)patients treated with voriconazole as a second-line therapy[6mg kg)1bid for2days,3mg kg)1IV twice daily(bid)for6–27days followed by oral 200mg day)1for up to24weeks].In the larger,randomised comparative trial of IA published by Herbrecht et al.[12],patients were treated with voriconazole(6mg kg)1IV bid on day1;4mg kg)1 bid for‡7days followed by oral voriconazole200mg bid) (n¼144)or with amphotericin B deoxycholate1.0–1.5mg kg)1day)1(n¼133).A complete or partial response was observed in32%and53%of patients treated with amphotericin B deoxycholate and voricon-azole respectively.Approximately one-third of these cases were included based on clinical and imaging criteria but without histologic or microbiologic confirmation of aspergillosis.For these cases that lacked microbiological confirmation,higher response rates were seen for both the voriconazole and amphotericin B deoxycholate groups(67.4%and42.9%respectively).This could represent a more favourable treatment effect associated with earlier intervention and/or lower fungal burdens. Recently,an open-label study of caspofungin as the second-line therapy was reported for83patients with proven or probable aspergillosis.14An overall(complete or partial)response was reported in45%of the83 patients.However,the overall response rate was only 14%in21allogeneic SCT recipients and26%in19 neutropenic patients.In the current analysis,an overall response was reported in32%of25patients treated with L-AMB as the second-line therapy.In the current pooled analysis,the underlying con-ditions resulting in immunosuppression were generally similar to those in the previously reported trials.12,13For example,in Herbrecht et al.[12]and Denning et al.[13]the number of patients who had undergone allogeneic SCT(20–26%),had acute leukaemia(35–45%),had solid organ transplantation(3–6%)or were infected with human immunodeficiency virus(4–5%)was gen-erally similar to the numbers in the current study.In addition,34(49%)patients were neutropenic at base-line in the current analysis,similar to that reported (45%)in the randomised study comparing voriconazole with amphotericin B deoxycholate12and substantially higher than the24%reported in the non-comparative trial of voriconazole.13Based on the patient populations and similar diagnostic criteria applied to document IFFI, the clinical response rate in this pooled analysis for L-AMB(51%)in proven or probable infection was higher than that reported for amphotericin B deoxych-olate(32%)and within the range of clinical response reported for voriconazole(48–53%)in the treatment of IA.It is important to note that L-AMB is active against Zygomycetes infections;however,voriconazole and caspofungin are not active against this family of organisms.Zygomycetes infections may be difficult to distinguish from Aspergillus infections clinically or via imaging;therefore,this limitation with voriconazole should be taken into consideration when treating patients with IFFI if microbiological confirmation of the fungal pathogen is lacking.In the current study,survival to the last follow-up visit in patients with proven or probable IFFI was51%, with66%of these patients surviving for‡12weeks. Because this analysis was a retrospective case review of patients from multiple clinical trials that followed different protocols,it is difficult to draw further conclu-sions from the survival data or compare the favourable results in this analysis to other more recently published trials.However,it is encouraging that more than half of the cases of proven or probable IFFI in a population of severely immunocompromised patients survived to the last follow-up visit.Table2Response rates according to doseand regimen.Dose(mg kg)1day)1)Patients(n)Overall response,n/n(%)1Response by dose regimen1169/16(56)Standard dose(1–5mg kg)1day)1)26/48(54%)2105/10(50)342/4(50)41327/13(54)553/5(60)7.542/4(50)High dose(>5mg kg)1day)1)9/21(43%)1052/5(40)12.553/5(60)1572/7(29)1Complete or partial response.2Median.C.Cordonnier et al.Journal CompilationÓ2007Blackwell Publishing Ltd•Mycoses(2007),50,205–209In conclusion,L-AMB has documented efficacy in the treatment of proven or probable IFFI in cases meeting current diagnostic criteria.Data from this retrospective analysis suggest an overall response rate(51%)that is comparable with voriconazole and higher than that of amphotericin B deoxycholate;however,these observa-tions have not been confirmed in randomised compa-rator trials.Furthermore,conclusions drawn from this study are limited in that it was a pooled analysis of selected studies that differed in drug dosage and diagnostic criteria.Despite these limitations,mounting evidence supports the role of AmBisome as an effective antifungal therapy.AcknowledgmentsThis work was supported by Gilead Sciences.References1Ellis D.Amphotericin B:spectrum and resistance.J Anti-microb Chemother2002;49(Suppl.1):7–10.2Walsh TJ,Finberg RW,Arndt C et al.Liposomal ampho-tericin B for empirical therapy in patients with persistent fever and neutropenia.National Institute of Allergy and Infectious Diseases Mycoses Study Group.N Engl J Med1999;340:764–71.3Leenders AC,Daenen S,Jansen RL et al.Liposomal amphotericin B compared with amphotericin B deoxych-olate in the treatment of documented and suspectedneutropenia-associated invasive fungal infections.Br JHaematol1998;103:205–12.4Ellis M,Spence D,de Pauw B et al.An EORTC interna-tional multicenter randomized trial(EORTC number19923)comparing two dosages of liposomal amphotericinB for treatment of invasive aspergillosis.Clin Infect Dis1998;27:1406–12.5Walsh TJ,Goodman JL,Pappas P et al.Safety,tolerance, and pharmacokinetics of high-dose liposomal amphoteri-cin B(AmBisome)in patients infected with Aspergillusspecies and other filamentous fungi:maximum tolerateddose study.Antimicrob Agents Chemother2001;45:3487–96.6Ringde´n O,Meunier F,Tollemar J et al.Efficacy of amphotericin B encapsulated in liposomes(AmBisome)in the treatment of invasive fungal infections in immuno-compromised patients.J Antimicrob Chemother1991;28: 73–82.7Tollemar J,Ringde´n O.Early pharmacokinetic and clinical results from a noncomparative multicentre trial ofamphotericin B encapsulated in a small unilamellar lipo-some(AmBisomeÒ).Drug Invest1992;4:232–8.8Mills W,Chopra R,Linch DC,Goldstone AH.Liposomal amphotericin B in the treatment of fungal infections inneutropenic patients:a single-centre experience of133episodes in116patients.Br J Haematol1994;86:754–60.9Ng TT,Denning DW.Liposomal amphotericin B(AmB-isome)therapy in invasive fungal infections.Evaluation of United Kingdom compassionate use data.Arch Intern Med 1995;155:1093–8.10Ascioglu S,Rex JH,de Pauw B et al.Defining opportunistic invasive fungal infections in immunocompromised pa-tients with cancer and hematopoietic stem cell trans-plants:an international consensus.Clin Infect Dis2002;34:7–14.11Cornely OA,Maertens J,Bresnik M,Herbrecht R.Lipo-somal amphotericin B(L-AMB)as initial therapy forinvasive filamentous fungal infections(IFFI):a random-ized,prospective trial of a high loading regimen vs.standard dosing(AmBiLoad Trial).Blood2005;106:900a(abstract3222).12Herbrecht R,Denning DW,Patterson TF et al.Voricon-azole versus amphotericin B for primary therapy of inva-sive aspergillosis.N Engl J Med2002;347:408–15.13Denning DW,Ribaud P,Milpied N et al.Efficacy and safety of voriconazole in the treatment of acute invasive asper-gillosis.Clin Infect Dis2002;34:563–71.14Maertens J,Raad I,Petrikkos G et al.Efficacy and safety of caspofungin for treatment of invasive aspergillosis in pa-tients refractory to or intolerant of conventional antifun-gal therapy.Clin Infect Dis2004;39:1563–71.Liposomal amphotericin B efficacyJournal CompilationÓ2007Blackwell Publishing Ltd•Mycoses(2007),50,205–209。