出院小结英文
- 格式:docx
- 大小:17.43 KB
- 文档页数:12
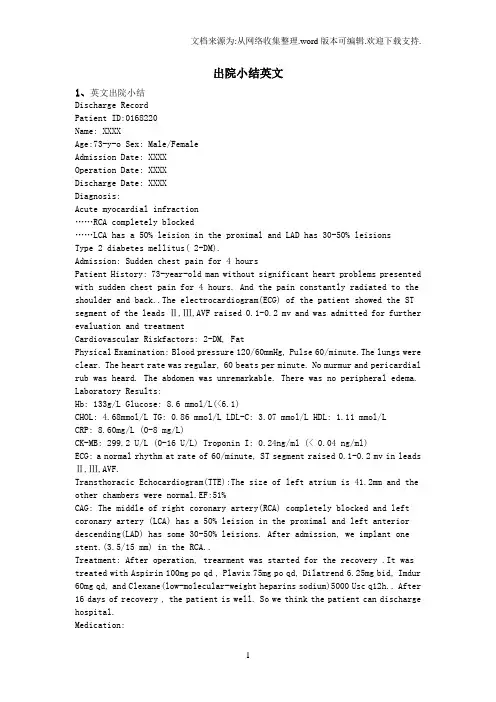
出院小结英文出院小结英文1、英文出院小结Discharge RecordPatient ID:0168220Name: XXXXAge:73-y-o Sex: Male/FemaleAdmission Date: XXXXOperation Date: XXXXDischarge Date: XXXXDiagnosis:Acute myocardial infraction……RCA completely blocked……LCA has a 50% leision in the proximal and LAD has 30-50% leisionsType 2 diabetes mellitus( 2-DM).Admission: Sudden chest pain for 4 hoursPatient History: 73-year-old man without significant heart problems presented with sudden chest pain for 4 hours. And the pain constantly radiated to the shoulder and back..The electrocardiogram(ECG) of the patient showed the ST segment of the leads Ⅱ,Ⅲ,AVF raised 0.1-0.2 mv and was admitted for further evaluation and treatmentCardiovascular Riskfactors: 2-DM, FatPhysical Examination: Blood pressure 120/60mmHg, Pulse 60/minute.The lungs were clear. The heart rate was regular, 60 beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. There was no peripheral edema.Laboratory Results:Hb: 133g/L Glucose: 8.6 mmol/L(<6.1)CHOL: 4.68mmol/L TG: 0.86 mmol/L LDL-C: 3.07 mmol/L HDL: 1.11 mmol/LCRP: 8.60mg/L (0-8 mg/L)CK-MB: 299.2 U/L (0-16 U/L) Troponin I: 0.24ng/ml (< 0.04 ng/ml)ECG: a normal rhythm at rate of 60/minute, ST segment raised 0.1-0.2 mv in leads Ⅱ,Ⅲ,AVF.Transthoracic Echocardiogram(TTE):The size of left atrium is 41.2mm and the other chambers were normal.EF:51%CAG: The middle of right coronary artery(RCA) completely blocked and left coronary artery (LCA) has a 50% leision in the proximal and left anterior descending(LAD) has some 30-50% leisions. After admission, we implant one stent.(3.5/15 mm) in the RCA..Treatment: After operation, trearment was started for the recovery .It was treated with Aspirin 100mg po qd , Plavix 75mg po qd, Dilatrend 6.25mg bid, Imdur 60mg qd, and Clexane(low-molecular-weight heparins sodium)5000 Uscq12h.. After 16 days of recovery , the patient is well. So we think the patient can discharge hospital.Medication:1.Medicines to improve heart function and their usesAspirin 100mg po 1-0-0Plavix 75mg po 1-0-0 for 9 monthsZocor(statin) 40mg po 0-0-1Micardis 40mg po 1-0-0Spironolactone 20mg po 1-0-0Dilatrend 6.25mg po 1-0-12.Medicines to control blood sugar and their usesGlargine(insulin) 34U ih 1-0-0Glucobay 50mg po 1-1-1Avandia 8mg po 1-0-0Comments:1. No smoking and drinking and keep diet2. Strictly controll blood sugar3. Be attention to keep rest and do not do high-intensity exercises4. Eat medicines on time and follow-up visit after one month. Dotor: XXXXXX2、英文出院小结姓名 Zhao XX 性别 male 年龄 51入院诊断 Acute pancreatitis简要病史、体格检查和入院辅助检查 Complaints:'left upper abdominal pain for 1 day.' alcohol triggered. severe, constant pain with nausea & vomiting. more intense when supine, but relieved by staying with the trunk flexed and knees drawn up. no radiation. no abdominal distention. no gallstone history. Physical examination: low-grade fever. normal to elevated BP. distressed, anxious. jaundice(-). moderate abdominal tenderness, with no musclerigidity. Laboratory data: serum amylase↑,serum lipase↑,urineamylase↑,white blood cells↑, plasma glucose↑. CT plaint scan: noindicative sign. gastroduodenal endoscopy: inflammatory changes, no ulcer observed. etc.治疗经过:fasting. intravenous fluids. nutritional support. nasogastric suction. prophylactic antibiotic. inhibiting pancreatic secretion. others including consultations.出院转归:resolution of abdominal pain出院诊断:Acute pancreatitis出院医嘱:avoidance of alcohol. fluid diet gradually to regular diet. symptoms observation. hospitalization when necessary.3、英文出院小结DICHARGE SUMMARYDISCHARGE DIAGNOSIS1. Unstable angina.2. Multi-vessel artery diease3. HyperlipidemaREASON FOR ADMISSIONMr.Zhou is a 69-year-old Chinese man who is actually a native of Beshing and in the United States visiting his daughter. he presented to the Heart Hospital emergency room with substernal discomfort radiating to the arm. There was mild improvement with nitroglycerin. He had discomfort on and off over a two-day period. He was admitted for further management.HOSPITAL COURSEMr.Zhou ruled out for a myocardial infarction by serial enzymes. An adenosine Cardiolite stress was performed. This showed anterior andinferior ischemia. Caridiac catheterization was then performed by Dr. Picone. Coronary arteriography revealed a subtotal proximal LAD followed by total occlusion mid vessel. The distal LAD filled via collaterals from the circumflex and looked small and diffusely diseased. The circumflex was patent. There was a 50 percent stenosis in the obtuse marginal. The right coronary artery had a 75 percent mid vessel stenosis and a 100 percent distal occlusion. There were right to right and left to right collaterals.Left ventriculography revealed an ejection fraction of 55 percent with anterior hypokinesis. Dr. Picone felt that he was not an ideal candidatefor bypass surgery and recommended medical management. Mr.Zhou was started on a combination of Imdur and metoprolol. Aspirin was continued. On April 26,20XX,he was still having low chest discomfort. It is difficult to get a complete story as the patient is Chinese speaking only, His daughter interpreted. I spent long periods with the family and describing the procedures and what was done and their implications. They will need to return to see Dr.Picone in two to three weeks.If he has more chest discomfort, then he may require surgical intervention.DISCHARGE MEDICATIONSMedications on discharge are Imdur 60 mg p.o.q.d.,metoprolol 25 mgp.o.b.i.d.,Lescol 40 mg p.o.q.d.,aspirin 325 mg p.o.q.d.,and Norvasc 2.5 mg p.o.q.d.FOLLOWUPFollow up with Dr.Picone in two to three weeks.4、出院小结name: 巴图吉亚age: 34sex: manmedical record number: 628848date of admission: 22.Dec.20XX.date of discharge: 6.Jan.20XXattending physician: zhangchengpingpresent history:8 years ago,he felt jaundice with no inducing factors,he first consulted local hospital,blood laboratories tests showed HBsAg ispositive,diagnosised as hepatitis B infection.he was given for treatment,and the liver function becomed normal.1 year ago,he was given interferon for treatment after injection 2 times,the treatment stoped forhigher ALT than before.since last year,he has taken intermittently pain in the upper abdomen after drunking.from the further treatment,he admitted to the liver disease department.prior to admission,he has examined liver function and other laboratories.(the result of test:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L).hospital course:after the patient`s hostitalization,he was started on heparolysate 100mg I.V.qd,shuganning(舒肝宁注射液) 30ml I.V.qd, compound glycyrrhizin 160mg I.V.qd,wuzhi jiaonang(五酯胶囊) 22.5mg P.O.t.i.d,and jianpi yishen keli(健脾益肾颗粒) 10g P.O.t.i.d.he responded very well to the therapy.up to now,he changes for the better and no obvious uncomfortable.Laboratory data:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L.White cell count ,hemoglobin ,hematocrit ,platelet count ,PT ,AFP mg/ml.admitting diagnosis:1.chronic viral hepatitis with HBV discharge diagnosis:1.chronic hepatitis B infection.2.liver cirrhosis(mild).Contition on discharge:Stable.discharge instructions:diet:home diet.Activity:as tolerated.Discharge Medications:Continued:1.wuzhi jiaonang(五酯胶囊) 22.5mg P.O.t.i.d.2.jianpi yishen keli(健脾益肾颗粒) 10g P.O.t.i.d. New:1.yinzhihuang keli(茵枝黄颗粒)6g P.O.t.i.d.Medical follow up1.follow up blood routine,prothrombin time(PT),liver function and a-fetoprotein(AFP) in 1 month.2.follow up HBV-marker,HBV-DNA,AFP and liver ultrasonograph every 6 month..signature:5、出院小结(外科)Medical CertificateName: ----- sex: male age:24 inpatient number:-------Inpatient date: from Aug.16,20XX to Sep.20 ,20XXDiagnosis:portal hypertension, liver cirrhosisCourse of treatment: First, we had a thorough examination for this patient,including physical examination, blood examination and image examination (All the data mentioned above had been copied by the patient).Then we had the diagnosis: portal hypertension, liver cirrhosis. And, in Aug.26,20XXwe underwent the operation:splenectomy with esophagus transection and anastomosis, and esophagogastric devascularization. After operationthe patient had got a basic recovery and was discharged on Sep.20 ,20XX. Instructions:1.It is suggested that he should rest for one month at home before resuming his work.2.See doctor and have some necessary examination regularly.3.See doctor anytime when feeling uncomfortable.Doctor in charge: Professor ----------20XX-10-9。
出院小结英文1、英文出院小结Discharge RecordPatient ID:0168220Name: XXXXAge:73-y-o Sex: Male/FemaleAdmission Date: XXXXOperation Date: XXXXDischarge Date: XXXXDiagnosis:Acute myocardial infraction……RCA completely b locked……LCA has a 50% leision in the proximal and LAD has 30-50% leisionsType 2 diabetes mellitus( 2-DM).Admission: Sudden chest pain for 4 hoursPatient History: 73-year-old man without significant heart problems presented with sudden chest pain for 4 hours. And the pain constantly radiated to the shoulder and back..The electrocardiogram(ECG) of the patient showed the ST segment of the leads Ⅱ,Ⅲ,AVF raised 0.1-0.2 mv and was admitted for further evaluation and treatmentCardiovascular Riskfactors: 2-DM, FatPhysical Examination: Blood pressure 120/60mmHg, Pulse 60/minute.The lungs were clear. The heart rate was regular, 60 beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. There was no peripheral edema.Laboratory Results:Hb: 133g/L Glucose: 8.6 mmol/L(<6.1)CHOL: 4.68mmol/L TG: 0.86 mmol/L LDL-C: 3.07 mmol/L HDL: 1.11 mmol/LCRP: 8.60mg/L (0-8 mg/L)CK-MB: 299.2 U/L (0-16 U/L) Troponin I: 0.24ng/ml (< 0.04 ng/ml)ECG: a normal rhythm at rate of 60/minute, ST segment raised 0.1-0.2 mv in leads Ⅱ,Ⅲ,AVF.Transthoracic Echocardiogram(TTE):The size of left atrium is 41.2mm and the other chambers were normal.EF:51%CAG: The middle of right coronary artery(RCA) completely blocked and left coronary artery (LCA) has a 50% leision in the proximal and left anterior descending(LAD) has some 30-50% leisions. After admission, we implant one stent.(3.5/15 mm) in the RCA..Treatment: After operation, trearment was started for the recovery .It was treated with Aspirin 100mg po qd , Plavix 75mg po qd, Dilatrend 6.25mg bid, Imdur 60mg qd, and Clexane(low-molecular-weight heparins sodium)5000 Usc q12h.. After 16 days of recovery , the patient is well. So we think the patient can discharge hospital.Medication:1.Medicines to improve heart function and their usesAspirin 100mg po 1-0-0Plavix 75mg po 1-0-0 for 9 monthsZocor(statin) 40mg po 0-0-1Micardis 40mg po 1-0-0Spironolactone 20mg po 1-0-0Dilatrend 6.25mg po 1-0-12.Medicines to control blood sugar and their usesGlargine(insulin) 34U ih 1-0-0Glucobay 50mg po 1-1-1Avandia 8mg po 1-0-0Comments:1. No smoking and drinking and keep diet2. Strictly controll blood sugar3. Be attention to keep rest and do not do high-intensity exercises4. Eat medicines on time and follow-up visit after one month.Dotor: XXXXXX2、英文出院小结姓名 Zhao XX 性别 male 年龄 51入院诊断 Acute pancreatitis简要病史、体格检查和入院辅助检查 Complaints:'left upper abdominal pain for 1 day.' alcohol triggered. severe, constant pain with nausea & vomiting. more intense when supine, but relieved by staying with the trunk flexed and kneesdrawn up. no radiation. no abdominal distention. no gallstone history. Physical examination: low-grade fever. normal to elevated BP. distressed, anxious. jaundice(-). moderate abdominal tenderness, with no muscle rigidity. Laboratory data: serum amylase↑,serum lipase↑,urine amylase↑,white blood cells↑, plasma glucose↑. CT plaint scan: no indicative sign. gastro duodenal endoscopy: inflammatory changes, no ulcer observed. etc.治疗经过:fasting. intravenous fluids. nutritional support. nasogastric suction. prophylactic antibiotic. inhibiting pancreatic secretion. others including consultations.出院转归:resolution of abdominal pain出院诊断:Acute pancreatitis出院医嘱:avoidance of alcohol. fluid diet gradually to regular diet. symptoms observation. hospitalization when necessary.3、英文出院小结DICHARGE SUMMARYDISCHARGE DIAGNOSIS1. Unstable angina.2. Multi-vessel artery diease3. HyperlipidemaREASON FOR ADMISSIONMr.Zhou is a 69-year-old Chinese man who is actually a native of Beshing and in the United States visiting his daughter. he presented to the Heart Hospital emergency room with substernal discomfort radiating to the arm. There was mild improvement with nitroglycerin. He had discomfort on and off over a two-day period. He was admitted for further management.HOSPITAL COURSEMr.Zhou ruled out for a myocardial infarction by serial enzymes. An adenosine Cardiolite stress was performed. This showed anterior and inferior ischemia. Caridiac catheterization was then performed by Dr. Picone. Coronary arteriography revealed a subtotal proximal LAD followed by total occlusion mid vessel. The distal LAD filled via collaterals from the circumflex and looked small and diffusely diseased. The circumflex was patent. There was a 50 percent stenosis in the obtuse marginal. The right coronary artery had a 75 percent mid vessel stenosis and a 100 percent distal occlusion. There were right to right and left to right collaterals. Left ventriculography revealed an ejection fraction of 55 percent with anterior hypokinesis. Dr. Picone felt that he was not an ideal candidate for bypass surgery and recommended medical management. Mr.Zhou was started on a combination of Imdur and metoprolol. Aspirin was continued. On April 26,20XX,he was still having low chest discomfort. It is difficult to get a complete story as the patient is Chinese speaking only, Hisdaughter interpreted. I spent long periods with the family and describing the procedures and what was done and their implications. They will need to return to see Dr.Picone in two to three weeks.If he has more chest discomfort, then he may require surgical intervention.DISCHARGE MEDICATIONSMedications on discharge are Imdur 60 mg p.o.q.d.,metoprolol 25 mgp.o.b.i.d.,Lescol 40 mg p.o.q.d.,aspirin 325 mg p.o.q.d.,and Norvasc 2.5 mg p.o.q.d.FOLLOWUPFollow up with Dr.Picone in two to three weeks.4、出院小结name: 巴图吉亚age: 34sex: manmedical record number: 628848date of admission: 22.Dec.20XX.date of discharge: 6.Jan.20XXattending physician: zhangchengpingpresent history:8 years ago,he felt jaundice with no inducing factors,he first consulted local hospital,blood laboratories tests showed HBsAg is positive,diagnosised as hepatitis B infection.he was given for treatment,and the liver function becomed normal.1 year ago,he was given interferon for treatment after injection 2 times,the treatment stoped for higher ALT than before.since last year,he has taken intermittently pain in the upper abdomen after drunking.from the further treatment,he admitted to the liver disease department.prior to admission,he has examined liver function and other laboratories.(the result of test:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L).hospital course:after the patient`s hostitalization,he was started on heparolysate 100mg I.V.qd,shuganning(舒肝宁注射液) 30ml I.V.qd, compound glycyrrhizin 160mg I.V.qd,wuzhi jiaonang(五酯胶囊) 22.5mg P.O.t.i.d,and jianpi yishen keli(健脾益肾颗粒) 10g P.O.t.i.d.he responded very well to the therapy.up to now,he changes for the better and no obvious uncomfortable.Laboratory data:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L.White cell count ,hemoglobin ,hematocrit ,platelet count ,PT ,AFP mg/ml.admitting diagnosis:1.chronic viral hepatitis with HBVdischarge diagnosis:1.chronic hepatitis B infection.2.liver cirrhosis(mild). Contition on discharge:Stable.discharge instructions:diet:home diet.Activity:as tolerated.Discharge Medications:Continued:1.wuzhi jiaonang(五酯胶囊) 22.5mg P.O.t.i.d.2.jianpi yishen keli(健脾益肾颗粒) 10g P.O.t.i.d. New:1.yinzhihuang keli(茵枝黄颗粒)6g P.O.t.i.d.Medical follow up1.follow up blood routine,prothrombin time(PT),liver function anda-fetoprotein(AFP) in 1 month.2.follow up HBV-marker,HBV-DNA,AFP and liver ultrasonograph every 6 month..signature:5、出院小结(外科)Medical CertificateName: ----- sex: male age:24 inpatient number:-------Inpatient date: from Aug.16,20XX to Sep.20 ,20XXDiagnosis:portal hypertension, liver cirrhosisCourse of treatment: First, we had a thorough examination for this patient, including physical examination, blood examination and image examination (All the data mentioned above had been copied by the patient).Then we hadthe diagnosis: portal hypertension, liver cirrhosis. And, in Aug.26,20XXwe underwent the operation:splenectomy with esophagus transection and anastomosis, and esophagogastric devascularization. After operationthe patient had got a basic recovery and was discharged on Sep.20 ,20XX.Instructions:1.It is suggested that he should rest for one month at home before resuming his work.2.See doctor and have some necessary examination regularly.3.See doctor anytime when feeling uncomfortable.Doctor in charge: Professor ----------20XX-10-9最新文件仅供参考已改成word文本。
出院小结英文1、英文出院小结Discharge RecordPatient ID:0168220Name: XXXXAge:73-y-o Sex: Male/FemaleAdmission Date: XXXXOperation Date: XXXXDischarge Date: XXXXDiagnosis:Acute myocardial infraction……RCA completely blocked……LCA has a 50% leision in the proxima l and LAD has 30-50% leisionsType 2 diabetes mellitus( 2-DM).Admission: Sudden chest pain for 4 hoursPatient History: 73-year-old man without significant heart problems presented with sudden chest pain for 4 hours. And the pain constantly radiated to the shoulder and back..The electrocardiogram(ECG) of the patient showed the ST segment of the leads Ⅱ,Ⅲ,AVF raised 0.1-0.2 mv and was admitted for further evaluation and treatmentCardiovascular Riskfactors: 2-DM, FatPhysical Examination: Blood pressure 120/60mmHg, Pulse 60/minute.The lungs were clear. The heart rate was regular, 60 beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. There was no peripheral edema. Laboratory Results:Hb: 133g/L Glucose: 8.6 mmol/L(<6.1)CHOL: 4.68mmol/L TG: 0.86 mmol/L LDL-C: 3.07 mmol/L HDL: 1.11 mmol/LCRP: 8.60mg/L (0-8 mg/L)CK-MB: 299.2 U/L (0-16 U/L) Troponin I: 0.24ng/ml (< 0.04 ng/ml)ECG: a normal rhythm at rate of 60/minute, ST segment raised 0.1-0.2 mv in leads Ⅱ,Ⅲ,AVF.Transthoracic Echocardiogram(TTE):The size of left atrium is 41.2mm and the other chambers were normal.EF:51%CAG: The middle of right coronary artery(RCA) completely blocked and left coronary artery (LCA) has a 50% leision in the proximal and left anterior descending(LAD) has some 30-50% leisions. After admission, we implant one stent.(3.5/15 mm) in the RCA..Treatment: After operation, trearment was started for the recovery .It was treated with Aspirin 100mg po qd , Plavix 75mg po qd, Dilatrend 6.25mg bid, Imdur 60mg qd, and Clexane(low-molecular-weight heparins sodium)5000 Usc q12h.. After 16 days of recovery , the patient is well. So we think the patient can discharge hospital.Medication:1.Medicines to improve heart function and their usesAspirin 100mg po 1-0-0Plavix 75mg po 1-0-0 for 9 monthsZocor(statin) 40mg po 0-0-1Micardis 40mg po 1-0-0Spironolactone 20mg po 1-0-0Dilatrend 6.25mg po 1-0-12.Medicines to control blood sugar and their usesGlargine(insulin) 34U ih 1-0-0Glucobay 50mg po 1-1-1Avandia 8mg po 1-0-0Comments:1. No smoking and drinking and keep diet2. Strictly controll blood sugar3. Be attention to keep rest and do not do high-intensity exercises4. Eat medicines on time and follow-up visit after one month.Dotor: XXXXXX2、英文出院小结姓名 Zhao XX 性别 male 年龄 51入院诊断 Acute pancreatitis简要病史、体格检查和入院辅助检查 Complaints:'left upper abdominal pain for 1 day.' alcohol triggered. severe, constant pain with nausea & vomiting. more intense when supine, but relieved by staying with the trunk flexed and knees drawn up. no radiation. no abdominal distention. no gallstone history. Physical examination: low-grade fever. normal to elevated BP. distressed, anxious. jaundice(-). moderate abdominal tenderness, with no muscle rigidity. Laboratory data: s erum amylase↑,serum lipase↑,urine amylase↑,white blood cells↑, plasma glucose↑. CT plaint scan: no indicative sign. gastroduodenal endoscopy: inflammatory changes, no ulcer observed. etc.治疗经过:fasting. intravenous fluids. nutritional support. nasogastric suction. prophylactic antibiotic. inhibiting pancreatic secretion. others including consultations.出院转归:resolution of abdominal pain出院诊断:Acute pancreatitis出院医嘱:avoidance of alcohol. fluid diet gradually to regular diet. symptoms observation. hospitalization when necessary.3、英文出院小结DICHARGE SUMMARYDISCHARGE DIAGNOSIS1. Unstable angina.2. Multi-vessel artery diease3. HyperlipidemaREASON FOR ADMISSIONMr.Zhou is a 69-year-old Chinese man who is actually a native of Beshing andin the United States visiting his daughter. he presented to the Heart Hospital emergency room with substernal discomfort radiating to the arm. There was mild improvement with nitroglycerin. He had discomfort on and off over a two-day period. He was admitted for further management.HOSPITAL COURSEMr.Zhou ruled out for a myocardial infarction by serial enzymes. An adenosine Cardiolite stress was performed. This showed anterior and inferior ischemia. Caridiac catheterization was then performed by Dr. Picone. Coronary arteriography revealed a subtotal proximal LAD followed by total occlusion mid vessel. The distal LAD filled via collaterals from the circumflex and looked small and diffusely diseased. The circumflex was patent. There was a 50 percent stenosis in the obtuse marginal. The right coronary artery had a 75 percent mid vessel stenosis and a 100 percent distal occlusion. There were right to right and left to right collaterals. Left ventriculography revealed an ejection fraction of 55 percent with anterior hypokinesis. Dr. Picone felt that he was not an ideal candidate for bypass surgery and recommended medical management. Mr.Zhou was started on a combination of Imdur and metoprolol. Aspirin was continued. On April 26,20XX,he was still having low chest discomfort. It is difficult to get a complete story as the patient is Chinese speaking only, His daughter interpreted. I spent long periods with the family and describing the procedures and what was done and their implications. They will need to return to see Dr.Picone in two to three weeks.If he has more chest discomfort, then he may require surgical intervention.DISCHARGE MEDICATIONSMedications on discharge are Imdur 60 mg ,metoprolol 25 mg ,Lescol 40 mg ,aspirin 325 mg ,and Norvasc 2.5 mgFOLLOWUPFollow up with Dr.Picone in two to three weeks.4、出院小结name: 巴图吉亚age: 34sex: manmedical record number: 628848date of admission:date of discharge:attending physician: zhangchengpingpresent history:8 years ago,he felt jaundice with no inducing factors,he first consulted local hospital,blood laboratories tests showed HBsAg is positive,diagnosised as hepatitis B infection.he was given for treatment,and the liver function becomed normal.1 year ago,he was given interferon for treatment after injection 2 times,the treatment stoped for higher ALT than before.since last year,he has taken intermittently pain in the upper abdomen after drunking.from the further treatment,he admitted to the liver disease department.prior to admission,he hasexamined liver function and other laboratories.(the result of test:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L).hospital course:after the patient`s hostitalization,he was started on heparolysate100mg ,shuganning(舒肝宁注射液) 30ml , compound glycyrrhizin 160mg ,wuzhi jiaonang(五酯胶囊) 22.5mg ,and jianpi yishen keli(健脾益肾颗粒) 10g responded very well to the therapy.up to now,he changes for the better and no obvious uncomfortable.Laboratory data:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L.White cell count ,hemoglobin ,hematocrit ,platelet count ,PT ,AFP mg/ml. admitting diagnosis:1.chronic viral hepatitis with HBVdischarge diagnosis:1.chronic hepatitis B infection.2.liver cirrhosis(mild).Contition on discharge:Stable.discharge instructions:diet:home diet.Activity:as tolerated.Discharge Medications:Continued:1.wuzhi jiaonang(五酯胶囊) 22.5mg2.jianpi yishen keli(健脾益肾颗粒) 10gNew:1.yinzhihuang keli(茵枝黄颗粒)6gMedical follow up1.follow up blood routine,prothrombin time(PT),liver function anda-fetoprotein(AFP) in 1 month.2.follow up HBV-marker,HBV-DNA,AFP and liver ultrasonograph every 6 month.. signature:5、出院小结(外科)Medical CertificateName: ----- sex: male age:24 inpatient number:-------Inpatient date: from Aug.16,20XX to Sep.20 ,20XXDiagnosis:portal hypertension, liver cirrhosisCourse of treatment: First, we had a thorough examination for this patient, including physical examination, blood examination and image examination (All the data mentioned above had been copied by the patient).Then we had the diagnosis: portal hypertension, liver cirrhosis. And, in Aug.26,20XXwe underwent the operation:splenectomy with esophagus transection and anastomosis, and esophagogastric devascularization. After operationthe patient had got a basic recovery and was discharged on Sep.20 ,20XX.Instructions:1.It is suggested that he should rest for one month at home before resuming his work.2.See doctor and have some necessary examination regularly.3.See doctor anytime when feeling uncomfortable.Doctor in charge: Professor ----------20XX-10-9。
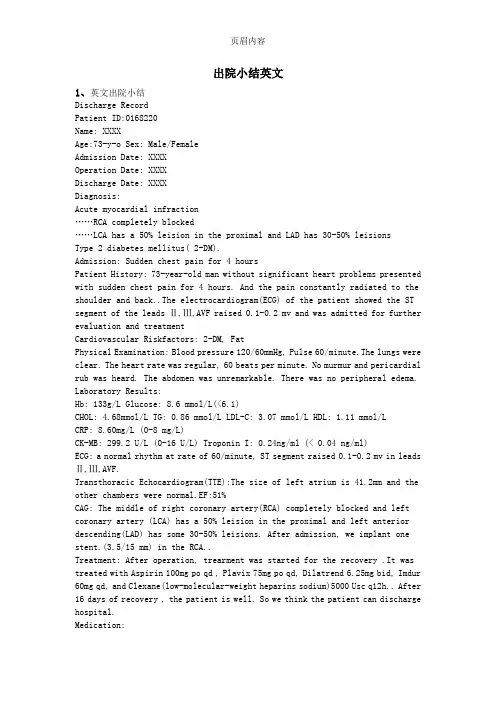
Discharge reportgynecology Bed number:15Name:LIN YUANBirth1962.6.5Gender:femaleAge:50 YNumber in hospital:Check-in time:2012-07-05 16:50:00 Check-out time:2012-07-07 14:00:00Days:2Outpatient endometrial diseasesHospital check endometrial diseasesDischarge check endometrial diseasesMain disease LIN YUAN,female,age 50,move in hospital by menstrual uncleaning。
No Abdominal pain,little colpo-blood,sleep well,fece and urine well。
Check:vulvae:(-),vulvae unhindered,and little Coffee object,cervix:nice。
Uterine precursor:slightly larger and hard,:In addition can see small piece of 3*3*3cm.Main Test results (July 6,in hospital)leucorrhea test nice. Blood coagulation、blood test、electrocardiogram test nice. Pregnancy tests (-);Liver and kidney’s electrolyte:normal;Infectious diseases:Hepatitis b core Ab(all),7.07S/CO,↑;Hepatitis b exteriorAb,14.55mIU/ml。
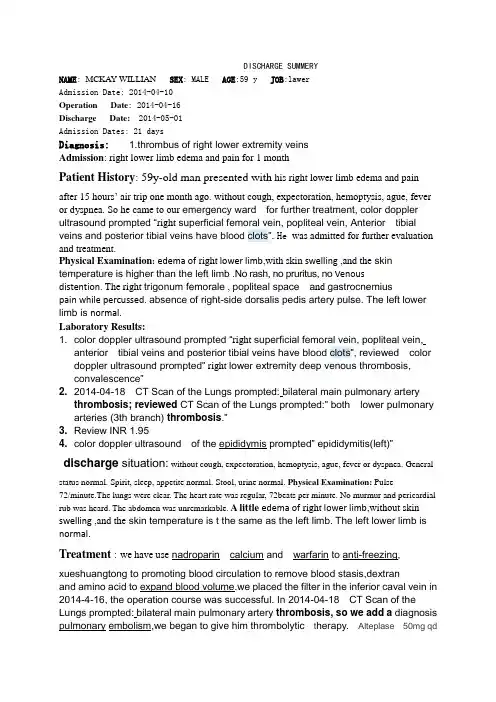
DISCHARGE SUMMERYNAME: MCKAY WILLIAN SEX: MALE AGE:59 y JOB:lawerAdmission Date: 2014-04-10Operation Date: 2014-04-16Discharge Date: 2014-05-01Admission Dates: 21 daysDiagnosis: 1.thrombus of right lower extremity veinsAdmission: right lower limb edema and pain for 1 monthPatient History: 59y-old man presented with his right lower limb edema and pain after 15 hours’ air trip one month ago. without cough, expectoration, hemoptysis, ague, fever or dyspnea. So he came to our emergency ward for further treatment, color doppler ultrasound prompted “right superficial femoral vein, popliteal vein, Anterior tibial veins and posterior tibial veins have blood clots”. He was admitted for further evaluation and treatment.Physical Examination:edema of right lower limb,with skin swelling ,and the skin temperature is higher than the left limb .No rash, no pruritus, no Venousdistention. The right trigonum femorale , popliteal space a nd gastrocnemiuspain while percussed. absence of right-side dorsalis pedis artery pulse. The left lower limb is normal.Laboratory Results:1. color doppler ultrasound prompted “right superficial femoral vein, popliteal vein,anterior tibial veins and posterior tibial veins have blood clots”, reviewed color doppler ultrasound prompted” right lower extremity deep venous thrombosis,convalescence”2. 2014-04-18 CT Scan of the Lungs prompted: bilateral main pulmonary arterythrombosis; reviewed CT Scan of the Lungs prompted:” both lower pulmonary arteries (3th branch) thrombosis.”3. Review INR 1.954. color doppler ultrasound of the epididymis prompted” epididymitis(left)”discharge situation:without cough, expectoration, hemoptysis, ague, fever or dyspnea. Generalstatus normal. Spirit, sleep, appetite normal. Stool, urine normal. Physical Examination: Pulse72/minute.The lungs were clear. The heart rate was regular, 72beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. A little edema of right lower limb,without skin swelling ,and the skin temperature is t the same as the left limb. The left lower limb is normal.Treatment : we have use nadroparin calcium and warfarin to anti-freezing, xueshuangtong to promoting blood circulation to remove blood stasis,dextranand amino acid to expand blood volume.we placed the filter in the inferior caval vein in 2014-4-16, the operation course was successful. In 2014-04-18 CT Scan of the Lungs prompted: bilateral main pulmonary artery thrombosis, so we add a diagnosis pulmonary embolism,we began to give him thrombolytic t herapy. Alteplase 50mg qdnow the INR is 1.95.discharge diagnosis:1.thrombus of right lower extremity veins 2. pulmonary embolism 3.epididymitis(left)∙Comments:1. No smoking and drinking and keep diet, don’t walk too much, don’t’ sit for a long time.2.Medicines to improve coagulation function ,keep INR 2~3:warfarin 2.5 pills qn.∙ 3. Follow-up clinic visit after one week。
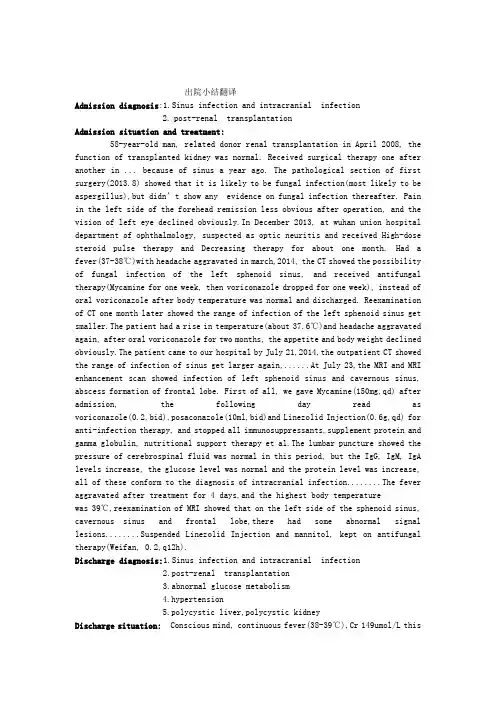
出院小结翻译Admission diagnosis:1.Sinus infection and intracranial infection2.post-renal transplantationAdmission situation and treatment:58-year-old man, related donor renal transplantation in April 2008, the function of transplanted kidney was normal. Received surgical therapy one after another in ... because of sinus a year ago. The pathological section of first surgery(2013.8) showed that it is likely to be fungal infection(most likely to be aspergillus),but didn’t show any evidence on fungal infection thereafter. Pain in the left side of the forehead remission less obvious after operation, and the vision of left eye declined obviously.In December 2013, at wuhan union hospital department of ophthalmology, suspected as optic neuritis and received High-dose steroid pulse therapy and Decreasing therapy for about one month. Had a fever(37-38℃)with headache aggravated in march,2014, the CT showed the possibility of fungal infection of the left sphenoid sinus, and received antifungal therapy(Mycamine for one week, then voriconazole dropped for one week), instead of oral voriconazole after body temperature was normal and discharged. Reexamination of CT one month later showed the range of infection of the left sphenoid sinus get smaller.The patient had a rise in temperature(about 37.6℃)and headache aggravated again, after oral voriconazole for two months, the appetite and body weight declined obviously.The patient came to our hospital by July 21,2014,the outpatient CT showed the range of infection of sinus get larger again,......At July 23,the MRI and MRI enhancement scan showed infection of left sphenoid sinus and cavernous sinus, abscess formation of frontal lobe. First of all, we gave Mycamine(150mg,qd) after admission, the following day read as voriconazole(0.2,bid),posaconazole(10ml,bid)and Linezolid Injection(0.6g,qd) for anti-infection therapy, and stopped all immunosuppressants,supplement protein and gamma globulin, nutritional support therapy et al.The lumbar puncture showed the pressure of cerebrospinal fluid was normal in this period, but the IgG, IgM, IgA levels increase, the glucose level was normal and the protein level was increase, all of these conform to the diagnosis of intracranial infection........The fever aggravated after treatment for 4 days,and the highest body temperaturewas 39℃,reexamination of MRI showed that on the left side of the sphenoid sinus, cavernous sinus and frontal lobe,there had some abnormal signal lesions........Suspended Linezolid Injection and mannitol, kept on antifungal therapy(Weifan, 0.2,q12h).Discharge diagnosis:1.Sinus infection and intracranial infection2.post-renal transplantation3.abnormal glucose metabolism4.hypertension5.polycystic liver,polycystic kidneyDischarge situation: Conscious mind, continuous fever(38-39℃),Cr 149umol/L thismorning........。
出院小结英文1、英文出院小结Discharge RecordPatient ID:0168220Name: XXXXAge:73-y-o Sex: Male/FemaleAdmission Date: XXXXOperation Date: XXXXDischarge Date: XXXXDiagnosis:Acute myocardial infraction……RCA completely blocked……LCA has a 50% leision in the proxima l and LAD has 30-50% leisionsType 2 diabetes mellitus( 2-DM).Admission: Sudden chest pain for 4 hoursPatient History: 73-year-old man without significant heart problems presented with sudden chest pain for 4 hours. And the pain constantly radiated to the shoulder and back..The electrocardiogram(ECG) of the patient showed the ST segment of the leads Ⅱ,Ⅲ,AVF raised 0.1-0.2 mv and was admitted for further evaluation and treatmentCardiovascular Riskfactors: 2-DM, FatPhysical Examination: Blood pressure 120/60mmHg, Pulse 60/minute.The lungs were clear. The heart rate was regular, 60 beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. There was no peripheral edema. Laboratory Results:Hb: 133g/L Glucose: 8.6 mmol/L(<6.1)CHOL: 4.68mmol/L TG: 0.86 mmol/L LDL-C: 3.07 mmol/L HDL: 1.11 mmol/LCRP: 8.60mg/L (0-8 mg/L)CK-MB: 299.2 U/L (0-16 U/L) Troponin I: 0.24ng/ml (< 0.04 ng/ml)ECG: a normal rhythm at rate of 60/minute, ST segment raised 0.1-0.2 mv in leads Ⅱ,Ⅲ,AVF.Transthoracic Echocardiogram(TTE):The size of left atrium is 41.2mm and the other chambers were normal.EF:51%CAG: The middle of right coronary artery(RCA) completely blocked and left coronary artery (LCA) has a 50% leision in the proximal and left anterior descending(LAD) has some 30-50% leisions. After admission, we implant one stent.(3.5/15 mm) in the RCA..Treatment: After operation, trearment was started for the recovery .It was treated with Aspirin 100mg po qd , Plavix 75mg po qd, Dilatrend 6.25mg bid, Imdur 60mg qd, and Clexane(low-molecular-weight heparins sodium)5000 Usc q12h.. After 16 days of recovery , the patient is well. So we think the patient can discharge hospital.Medication:1.Medicines to improve heart function and their usesAspirin 100mg po 1-0-0Plavix 75mg po 1-0-0 for 9 monthsZocor(statin) 40mg po 0-0-1Micardis 40mg po 1-0-0Spironolactone 20mg po 1-0-0Dilatrend 6.25mg po 1-0-12.Medicines to control blood sugar and their usesGlargine(insulin) 34U ih 1-0-0Glucobay 50mg po 1-1-1Avandia 8mg po 1-0-0Comments:1. No smoking and drinking and keep diet2. Strictly controll blood sugar3. Be attention to keep rest and do not do high-intensity exercises4. Eat medicines on time and follow-up visit after one month.Dotor: XXXXXX2、英文出院小结姓名 Zhao XX 性别 male 年龄 51入院诊断 Acute pancreatitis简要病史、体格检查和入院辅助检查 Complaints:'left upper abdominal pain for 1 day.' alcohol triggered. severe, constant pain with nausea & vomiting. more intense when supine, but relieved by staying with the trunk flexed and knees drawn up. no radiation. no abdominal distention. no gallstone history. Physical examination: low-grade fever. normal to elevated BP. distressed, anxious. jaundice(-). moderate abdominal tenderness, with no muscle rigidity. Laboratory data: s erum amylase↑,serum lipase↑,urine amylase↑,white blood cells↑, plasma glucose↑. CT plaint scan: no indicative sign. gastroduodenal endoscopy: inflammatory changes, no ulcer observed. etc.治疗经过:fasting. intravenous fluids. nutritional support. nasogastric suction. prophylactic antibiotic. inhibiting pancreatic secretion. others including consultations.出院转归:resolution of abdominal pain出院诊断:Acute pancreatitis出院医嘱:avoidance of alcohol. fluid diet gradually to regular diet. symptoms observation. hospitalization when necessary.3、英文出院小结DICHARGE SUMMARYDISCHARGE DIAGNOSIS1. Unstable angina.2. Multi-vessel artery diease3. HyperlipidemaREASON FOR ADMISSIONMr.Zhou is a 69-year-old Chinese man who is actually a native of Beshing andin the United States visiting his daughter. he presented to the Heart Hospital emergency room with substernal discomfort radiating to the arm. There was mild improvement with nitroglycerin. He had discomfort on and off over a two-day period. He was admitted for further management.HOSPITAL COURSEMr.Zhou ruled out for a myocardial infarction by serial enzymes. An adenosine Cardiolite stress was performed. This showed anterior and inferior ischemia. Caridiac catheterization was then performed by Dr. Picone. Coronary arteriography revealed a subtotal proximal LAD followed by total occlusion mid vessel. The distal LAD filled via collaterals from the circumflex and looked small and diffusely diseased. The circumflex was patent. There was a 50 percent stenosis in the obtuse marginal. The right coronary artery had a 75 percent mid vessel stenosis and a 100 percent distal occlusion. There were right to right and left to right collaterals. Left ventriculography revealed an ejection fraction of 55 percent with anterior hypokinesis. Dr. Picone felt that he was not an ideal candidate for bypass surgery and recommended medical management. Mr.Zhou was started on a combination of Imdur and metoprolol. Aspirin was continued. On April 26,20XX,he was still having low chest discomfort. It is difficult to get a complete story as the patient is Chinese speaking only, His daughter interpreted. I spent long periods with the family and describing the procedures and what was done and their implications. They will need to return to see Dr.Picone in two to three weeks.If he has more chest discomfort, then he may require surgical intervention.DISCHARGE MEDICATIONSMedications on discharge are Imdur 60 mg ,metoprolol 25 mg ,Lescol 40 mg ,aspirin 325 mg ,and Norvasc 2.5 mgFOLLOWUPFollow up with Dr.Picone in two to three weeks.4、出院小结name: 巴图吉亚age: 34sex: manmedical record number: 628848date of admission:date of discharge:attending physician: zhangchengpingpresent history:8 years ago,he felt jaundice with no inducing factors,he first consulted local hospital,blood laboratories tests showed HBsAg is positive,diagnosised as hepatitis B infection.he was given for treatment,and the liver function becomed normal.1 year ago,he was given interferon for treatment after injection 2 times,the treatment stoped for higher ALT than before.since last year,he has taken intermittently pain in the upper abdomen after drunking.from the further treatment,he admitted to the liver disease department.prior to admission,he hasexamined liver function and other laboratories.(the result of test:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L).hospital course:after the patient`s hostitalization,he was started on heparolysate100mg ,shuganning(舒肝宁注射液) 30ml , compound glycyrrhizin 160mg ,wuzhi jiaonang(五酯胶囊) 22.5mg ,and jianpi yishen keli(健脾益肾颗粒) 10g responded very well to the therapy.up to now,he changes for the better and no obvious uncomfortable.Laboratory data:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L.White cell count ,hemoglobin ,hematocrit ,platelet count ,PT ,AFP mg/ml. admitting diagnosis:1.chronic viral hepatitis with HBVdischarge diagnosis:1.chronic hepatitis B infection.2.liver cirrhosis(mild).Contition on discharge:Stable.discharge instructions:diet:home diet.Activity:as tolerated.Discharge Medications:Continued:1.wuzhi jiaonang(五酯胶囊) 22.5mg2.jianpi yishen keli(健脾益肾颗粒) 10gNew:1.yinzhihuang keli(茵枝黄颗粒)6gMedical follow up1.follow up blood routine,prothrombin time(PT),liver function anda-fetoprotein(AFP) in 1 month.2.follow up HBV-marker,HBV-DNA,AFP and liver ultrasonograph every 6 month.. signature:5、出院小结(外科)Medical CertificateName: ----- sex: male age:24 inpatient number:-------Inpatient date: from Aug.16,20XX to Sep.20 ,20XXDiagnosis:portal hypertension, liver cirrhosisCourse of treatment: First, we had a thorough examination for this patient, including physical examination, blood examination and image examination (All the data mentioned above had been copied by the patient).Then we had the diagnosis: portal hypertension, liver cirrhosis. And, in Aug.26,20XXwe underwent the operation:splenectomy with esophagus transection and anastomosis, and esophagogastric devascularization. After operationthe patient had got a basic recovery and was discharged on Sep.20 ,20XX.Instructions:1.It is suggested that he should rest for one month at home before resuming his work.2.See doctor and have some necessary examination regularly.3.See doctor anytime when feeling uncomfortable.Doctor in charge: Professor ----------20XX-10-9。
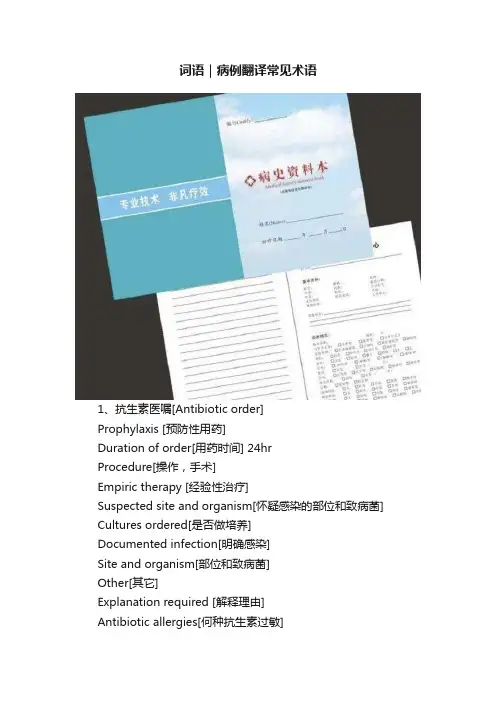
词语|病例翻译常见术语1、抗生素医嘱[Antibiotic order]Prophylaxis [预防性用药]Duration of order[用药时间] 24hrProcedure[操作,手术]Empiric therapy [经验性治疗]Suspected site and organism[怀疑感染的部位和致病菌] Cultures ordered[是否做培养]Documented infection[明确感染]Site and organism[部位和致病菌]Other[其它]Explanation required [解释理由]Antibiotic allergies[何种抗生素过敏]No known allergy [无已知的过敏]Drug+ dose+ Route+ frequency[药名+剂量+途径+次数] 2、医嘱首页[Admission / transfer]Admit / transfer to [收入或转入]Resident [住院医师] Attending[主治医师]Condition [病情]Diagnosis[诊断]Diet [饮食]Activity [活动]Vital signs[测生命体征]I / O [记进出量]Allergies[过敏]3、住院病历[case history]Identification [病人一般情况]Name[性名]Sex[性别]Age [年龄]Marriage[婚姻]Person to notify and phone No.[联系人及电话]Race[民族]I.D. No.[身份证]Admission date[入院日期]Source of history[病史提供者]Reliability of history[可靠程度]Medical record No[病历号]Business phone No.[工作单位电话]Home address and phone No.[家庭住地及电话]Chief complaint[主诉]History of present illness[现病史]Past History[过去史]Surgical[外科]Medical[内科]Medications[用药]Allergies[过敏史]Social History[社会史]Habits[个人习惯]Smoking[吸烟]Family History[家族史]Ob/Gyn History[ 婚姻/生育史]Alcohol use[喝酒]Review of Aystems[系统回顾]General[概况]Eyes, Ears, Nose and throat[五官] Pulmonary[呼吸]Cardiovascular[心血管]GI[消化]GU[生殖、泌尿系统]Musculoskeletal[肌肉骨骼]Neurology[神经系统]Endocrinology[内分泌系统]Lymphatic/Hematologic[淋巴系统/血液系统] Physical Exam[体检]Vital Signs[生命体征]lP[脉博]Bp[血压]R[呼吸]T[温度]Height[身高]Weight[体重]General[概况]lHEENT[五官]Neck[颈部]Back/Chest[背部/胸部]Breast[乳房]Heart[心脏]lHeart rate[心率]Heart rhythm[心律]Heart Border[心界]Murmur[杂音]Abdomen[腹部]lLiver[肝]Spleen[脾]Rectal[直肠]Genitalia[生殖系统]Extremities[四肢]lNeurology[神经系统]cranial nerves[颅神经]sensation[感觉]Motor[运动]Special P.E. on diseased organ system[专科情况] Radiographic Findings[放射]Laboratory Findings[化验]Assessment[初步诊断与诊断依据]Summary[病史小结]Treatment Plan[治疗计划]4、输血申请单[Blood bank requisition form] (1)reason for infusion[输血原因]红细胞[packed red cells, wshed RBCs]:*Hb<8.5>8.5><>*>20% blood volume lost [>20%血容量丢失]*cardio-pulmonary bypass with anticipated Hb [心肺分流术伴预计血色素 ]*chemotherapy or surgery with Hb <><>全血[whole blood]:massive on-going blood loss[大量出血]血小板[platelets]:*massive blood transfusion >10 units[输血10单位以上者]*platelet cou nt <50×103 l="" with="" active="" bleeding="" or="">50×103><>*Cardio-pulmonary bypass uith pl<100×103 lwith="" octive="">100×103><>*Platelet count <20×103>20×103><>新鲜冰冻血浆[fresh frozen plasma]:*documented abnormal PT or PTT with bleeding orSurgery[PT、PTT异常的出血或手术病人]*specific clotting factor deficiencies with bleeding/surgerg[特殊凝血因子缺乏的出血/手术者]*blood transfusion >15units[输血>15个单位]*warfarin or antifibrinolytic therapy withbleeding[华法令或溶栓治疗后出血]*DIC[血管内弥漫性凝血]*Antithrombin III dficiency[凝血酶III 缺乏](2)输血要求[request for blood components]*patient blood group[血型]*Has the patient had transfusion or pregnancy in the past 3 months? [近3个月,病人是否输过血或怀孕过?]*Type and crossmatch [血型和血交叉]*Units or ml[单位或毫升]5、出院小结[discharge summary]Patient Name[病人姓名]lMedical Record No.[病历号]lAttending Physician[主治医生]lDate of Admission[入院日期]lDate of Discharge[出院日期]lPrincipal Diagnosis[主要诊断]lSecondary Diagnosis[次要诊断]lComplications[并发症]lOperation[手术名称]lReason for Admission[入院理由]lPhysical Findings[阳性体征]lLab/X-ray Findings[化验及放射报告]lHospital Course[住院诊治经过]lCondition[出院状况]lDisposition[出院去向]lMedications[出院用药]lPrognosis[预后]lSpecial Instruction to the Patient(diet,physical activity)[出院指导(饮食,活动量)]lFollow-up Care[随随访]l6、住院/出院病历首页[Admission/discharge record]Patient name[病人姓名]race[种族]address[地址]religion[宗教]medical service[科别]admit (discharge) date[入院(出院)日期]Length of stay [住院天数]guarantor name [担保人姓名]next of kin or person to notify[需通知的亲属姓名]relation to the patient[与病人关系]previous admit date[上次住院日期]admitting physician [入院医生]attending physician [主治医生]admitting diagnosis[入院诊断]final (principal) diagnosis[最终(主要)诊断]secondary diagnosis[次要诊断]adverse reactions (complications)[副作用(合并症)]incision type[切口类型]healing course[愈合等级]operative (non-operative) procedures[手术(非手术)操作] nosocomial infection[院内感染]consultants [会诊]Critical-No. of times[抢救次数]recovered-No. of times[成功次数]Diagnosis qualitative analysis[诊断质量]OP.adm.and discharge Dx concur [门诊入院与出院诊断符合率] Clinical and pathological Dx concur[临床与病理诊断符合率]Pre- and post-operative Dx concur [术前术后诊断符合率]Dx determined with in 24 hours (3 days) afteradmission[入院后24小时(3 天)内确诊]Discharge status[出院状况]recovered[治愈]improved[好转]not improved[未愈]died [死亡]Dispositon[去向]home[家]against medical ad[自动出院]autosy[尸检]transferred to[转院到]本文转自:华译翻译。
出院小结英文作文I'm finally out of the hospital! It feels so good to be back home and out of that sterile, fluorescent-lit room. I can't wait to sleep in my own bed and take a long, hot shower. No more hospital food for me – I'm craving a big, juicy burger and some crispy fries.The doctors and nurses were amazing. They took such good care of me and made sure I was comfortable the whole time. I'll never forget the kindness and compassion they showed me during my stay. I'm so grateful for all their hard work and dedication.I'm still a bit weak and tired, but I know I'll get back to my old self soon. I have to take it easy for a while and let my body heal, but I'm looking forward to getting back to my normal routine. I miss going for walksin the park and meeting up with friends for coffee.I have to remember to take my medication and follow allthe doctor's orders. It's important to stay on top of my recovery and not push myself too hard. I don't want to end up back in the hospital, that's for sure.I'm going to make sure to keep in touch with thefriends I made in the hospital. We went through a lot together, and I know we'll always have a special bond. It's comforting to know that I have their support as I continue on the road to recovery.。
英文出院报告作文模版英文:I am pleased to report that I am being discharged from the hospital today. My condition has improved significantly since I was admitted, and I am feeling much better now.During my stay, I received excellent care from the medical staff. They were very attentive and responsive to my needs, and I felt well taken care of at all times. The nurses in particular were very kind and compassionate, and they made me feel comfortable and at ease.I also appreciated the various amenities and services available at the hospital. The food was surprisingly good, and I was able to watch TV and use the internet to pass the time. The hospital was clean and well-maintained, which helped to create a pleasant and welcoming environment.Overall, I am very grateful for the care and attentionI received during my stay at the hospital. I would like to thank all of the medical staff for their hard work and dedication, and I wish them all the best in their future endeavors.中文:我很高兴地报告,我今天被医院出院了。
出院小结英文作文I'm finally out of the hospital! It feels so good to be back home and away from all the beeping machines andsterile smells. I can't wait to sleep in my own bed and eat real food again.The doctors and nurses were really nice, but I'm gladto be done with all the poking and prodding. I never wantto see another needle again in my life. And those hospital gowns? They are the worst.I'm feeling a lot better now, but I know I still haveto take it easy for a while. The doctor gave me a bunch of prescriptions to fill and some instructions to follow. I guess I'll have to be responsible for a little while longer.I want to thank all my friends and family for visiting me while I was in the hospital. It really meant a lot to have their support during such a tough time. I don't know what I would have done without them.I'm looking forward to getting back to my normal routine, but I know it's going to take some time. I have to be patient with myself and not push too hard. It's going to be a slow process, but I'm ready for the challenge.Overall, I'm just grateful to be on the road to recovery. I know I still have a long way to go, but I'm determined to get there. I'm going to take things one day at a time and focus on getting better.。
出院小结英文5篇英文出院小结Discharge RecordPatient ID:0168220Name: xxAge:73-y-o Sex: Male/FemaleAdmission Date: xxOperation Date: xxDischarge Date: xxDiagnosis:Acute myocardial infraction……RCA pletely blocked……LCA has a 50% leision in the prox imal and LAD has 30-50% leisionsType 2 diabetes mellitus( 2-DM).Admission: Sudden chest pain for 4 hoursPatient History: 73-year-old man without significant heart problems presented with sudden chest pain for 4 hours. And the pain constantly radiated to the shoulder and back..The electrocardiogram(ECG) of thepatient showed the ST segment of the leads Ⅱ,Ⅲ,A VF raised 0.1-0.2 mv and was admitted for further evaluation and treatmentCardiovascular Riskfactors: 2-DM, FatPhysical Examination: Blood pressure 120/60mmHg, Pulse 60/minute.The lungs were clear. The heart rate was regular, 60 beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. There was no peripheral edema.Laboratory Results:Hb: 133g/L Glucose: 8.6 mmol/L(<6.1)CHOL:4.68mmol/L TG: 0.86 mmol/L LDL-C:3.07 mmol/L HDL:1.11 mmol/LCRP: 8.60mg/L (0-8 mg/L)CK-MB: 299.2 U/L (0-16 U/L) Troponin I: 0.24ng/ml (< 0.04 ng/ml) ECG: a normal rhythm at rate of 60/minute, ST segment raised 0.1-0.2 mv in leads Ⅱ,Ⅲ,A VF.Transthoracic Echocardiogram(TTE):The size of left atrium is 41.2mm and the other chambers were normal.EF:51%CAG: The middle of right coronary artery(RCA) pletely blocked and left coronary artery (LCA) has a 50% leision in the proximal and left anteriordescending(LAD) has some 30-50% leisions. After admission, we implant one stent.(3.5/15 mm) in the RCA..Treatment: After operation, trearment was started for the recovery .It was treated with Aspirin 100mg po qd , Plavix 75mg po qd, Dilatrend6.25mg bid, Imdur 60mg qd, and Clexane(low-molecular-weight heparxx sodium)5000 Usc q12h.. After 16 days of recovery , the patient is well. So we think the patient can discharge hospital.Medication:1.Medicines to improve heart function and their usesAspirin 100mg po 1-0-0Plavix 75mg po 1-0-0 for 9 monthsZocor(statin) 40mg po 0-0-1Micardis 40mg po 1-0-0Spironolactone 20mg po 1-0-0Dilatrend6.25mg po 1-0-12.Medicines to control blood sugar and their usesGlargine(xxulin) 34U ih 1-0-0Glucobay 50mg po 1-1-1Avandia 8mg po 1-0-0ments:1. No smoking and drinking and keep diet2. Strictly controll blood sugar3. Be attention to keep rest and do not do high-intensity exercises4. Eat medicines on time and follow-up visit after one month.Dotor: xx英文出院小结姓名Zhao xx 性别male 年龄51入院诊断Acute pancreatitis简要病史、体格检查和入院辅助检查plaints:”left upper abdominal pain for 1 day.” alcohol triggered. severe, constant pain with nausea & vomiting. more intense when supine, but relieved by staying with the trunk flexed and knees drawn up. no radiation. no abdominal distention. no gallstone history. Physical examination: low-grade fever. normal to elevated BP. distressed, anxious. jaundice(-). moderate abdominal tenderness, with no muscle rigidity. Laboratory data: serumamylase↑,serum lipase↑,urine amylase↑,white blood cells↑, plasma glucose↑. CT plaint scan: no indicative sign. gastroduodenal endoscopy: inflammatory changes, no ulcer observed. etc.治疗经过:fasting. intravenous fluids. nutritional support. nasogastric suction. prophylactic antibiotic. inhibiting pancreatic secretion. others including consultations.出院转归:resolution of abdominal pain出院诊断:Acute pancreatitis出院医嘱:avoidance of alcohol. fluid diet gradually to regular diet. symptoms observation. hospitalization when necessary.英文出院小结DICHARGE SUMMARYDISCHARGE DIAGNOSIS1. Unstable angina.2. Multi-vessel artery diease3. HyperlipidemaREASON FOR ADMISSIONMr.Zhou is a 69-year-old Chinese man who is actually a native of Beshing and in the United States visiting his daughter. he presented to the Heart Hospital emergency room with substernal disfort radiating to the arm. There was mild improvement with nitroglycerin. He had disfort on and off over a two-day period. He was admitted for further management.HOSPITAL COURSEMr.Zhou ruled out for a myocardial infarction by serial enzymes. An adenosine Cardiolite stress was performed. This showed anterior and inferior ischemia. Caridiac catheterization was then performed by Dr. Picone. Coronary arteriography revealed a subtotal proximal LAD followed by total occlusion mid vessel. The distal LAD filled via collaterals from the circumflex and looked small and diffusely diseased. The circumflex was patent. There was a 50 percent stenosis in the obtuse marginal. The right coronary artery had a 75 percent mid vessel stenosis and a 100 percent distal occlusion. There were right to right and left to right collaterals. Left ventriculography revealed an ejection fraction of 55 percent with anterior hypokinesis. Dr. Picone felt that he was not an ideal candidate for bypass surgery and remended medical management.Mr.Zhou was started on a bination of Imdur and metoprolol. Aspirin was continued. On April 26,xx,he was still having low chest disfort. It is difficult to get a plete story as the patient is Chinese speaking only, His daughter interpreted. I spent long periods with the family and describing the procedures and what was done and their implications. They will need to return to see Dr.Picone in two to three weeks.If he has more chest disfort, then he may require surgical intervention.DISCHARGE MEDICATIONSMedications on discharge are Imdur 60 mg p.o.q.d.,metoprolol 25 mg p.o.b.i.d.,Lescol 40 mg p.o.q.d.,aspirin 325 mg p.o.q.d.,and Norvasc2.5 mg p.o.q.d.FOLLOWUPFollow up with Dr.Picone in two to three weeks.出院小结name: 巴图吉亚age: 34sex: manmedical record number: 628848date of admission: 22.Dec.xx.date of discharge:6.Jan.xxattending physician: zhangchengpingpresent history:8 years ago,he felt jaundice with no inducing factors,he first consulted local hospital,blood laboratories tests showed HBsAg is positive,diagnosised as hepatitis B infection.he was given for treatment,and the liver function beed normal.1 year ago,he was given interferon for treatment after injection 2 times,the treatment stoped for higher ALT than before.since last year,he has taken intermittently pain in the upper abdomen after drunking.from the further treatment,he admitted to the liver disease department.prior to admission,he has examined liver function and other laboratories.(the result of test:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L).hospital course:after the patient`s hostitalization,he was started on heparolysate 100mg I.V.qd,shuganning(舒肝宁注射液) 30ml I.V.qd, pound glycyrrhizin 160mg I.V.qd,wuzhi jiaonang(五酯胶囊) 22.5mg P.O.t.i.d,and jianpi yishen keli(健脾益肾颗粒) 10g P.O.t.i.d.he responded very well to the therapy.up to now,he changes for the better and no obvious unfortable.Laboratory data:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L.White cell count ,hemoglobin ,hematocrit ,platelet count ,PT ,AFP mg/ml.admitting diagnosis:1.chronic viral hepatitis with HBVdischarge diagnosis:1.chronic hepatitis B infection.2.liver cirrhosis(mild). Contition on discharge: Stable.discharge xxtructions:diet:home diet.Activity:as tolerated. Discharge Medications: Continued:1.wuzhi jiaonang(五酯胶囊) 22.5mg P.O.t.i.d.2.jianpi yishen keli(健脾益肾颗粒) 10g P.O.t.i.d.New:1.yinzhihuang keli(茵枝黄颗粒)6g P.O.t.i.d.Medical follow up1.follow up blood routine,prothrombin time(PT),liver function and a-fetoprotein(AFP) in 1 month.2.follow up HBV-marker,HBV-DNA,AFP and liver ultrasonograph every 6 month..signature:出院小结(外科)Medical CertificateName: ----- sex: male age:24 inpatient number:-------Inpatient date: from Aug.16,xx to Sep.20 ,xxDiagnosis:portal hypertension, liver cirrhosisCourse of treatment: First, we had a thorough examination for this patient,including physical examination, blood examination and image examination(All the data mentioned above had been copied by the patient).Then we hadthe diagnosis: portal hypertension, liver cirrhosis. And, in Aug.26,xxwe underwent the operation:splenectomy with esophagus transection and anastomosis, and esophagogastric devascularization. After operationthe patient had got a basic recovery and was discharged on Sep.20 ,xx. xxtructions:1.It is suggested that he should rest for one month at home before resuming his work.2.See doctor and have some necessary examination regularly.3.See doctor anytime when feeling unfortable.Doctor in charge: Professor ----------xx-10-9。
英文出院小结作文英文:After spending a few days in the hospital, I am now being discharged. Overall, my experience here has been positive. The medical staff were very professional and attentive, and I received excellent care.During my stay, I underwent a few tests and procedures to determine the cause of my illness. The doctors were thorough in their examinations and explained everything to me in a clear and concise manner. They also took the time to answer any questions that I had.One thing that really stood out to me was the kindness and compassion shown by the nurses. They were always checking on me and making sure that I was comfortable. They also went out of their way to make me feel at ease, which helped to alleviate some of the anxiety that comes with being in a hospital.Now that I am being discharged, the doctors have given me some instructions to follow to ensure a smooth recovery.I need to take my medication as prescribed, get plenty of rest, and follow a healthy diet. I also need to attendfollow-up appointments to monitor my progress.Overall, I am grateful for the care that I received during my stay in the hospital. I feel confident that Iwill make a full recovery with the help of the medicalstaff and the support of my loved ones.中文:在医院待了几天之后,我现在要出院了。
DISCHARGE SUMMERYNAME: MCKAY WILLIAN SEX: MALE AGE:59 y JOB:lawerAdmission Date: 2014-04-10Operation Date: 2014-04-16Discharge Date: 2014-05-01Admission Dates: 21 daysDiagnosis: 1.thrombus of right lower extremity veinsAdmission: right lower limb edema and pain for 1 monthPatient History: 59y-old man presented with his right lower limb edema and painafter 15 hours’ air trip one month ago. without cough, expectoration, hemoptysis, ague, fever or dyspnea. So he came to our emergency ward for further treatment, color doppler ultrasound prompted “right superficial femoral vein, popliteal vein, Anterior tibial veins and posterior tibial veins have blood clots”. He was admitted for further evaluation and treatment.Physical Examination:edema of right lower limb,with skin swelling ,and the skin temperature is higher than the left limb .No rash, no pruritus, no Venousdistention. The right trigonum femorale , popliteal space a nd gastrocnemiuspain while percussed. absence of right-side dorsalis pedis artery pulse. The left lower limb is normal.Laboratory Results:1. color doppler ultrasound prompted “right superficial femoral vein, popliteal vein,anterior tibial veins and posterior tibial veins have blood clots”, reviewed color doppler ultrasound prompted” right lower extremity deep venous thrombosis,convalescence”2. 2014-04-18 CT Scan of the Lungs prompted: bilateral main pulmonary arterythrombosis; reviewed CT Scan of the Lungs prompted:” both lower pulmonary arteries (3th branch) thrombosis.”3. Review INR 1.954. color doppler ultrasound of the epididymis prompted” epididymitis(left)”discharge situation:without cough, expectoration, hemoptysis, ague, fever or dyspnea. Generalstatus normal. Spirit, sleep, appetite normal. Stool, urine normal. Physical Examination: Pulse72/minute.The lungs were clear. The heart rate was regular, 72beats per minute. No murmur and pericardial rub was heard. The abdomen was unremarkable. A little edema of right lower limb,without skin swelling ,and the skin temperature is t the same as the left limb. The left lower limb is normal.Treatment : we have use nadroparin calcium and warfarin to anti-freezing, xueshuangtong to promoting blood circulation to remove blood stasis,dextranand amino acid to expand blood volume.we placed the filter in the inferior caval vein in 2014-4-16, the operation course was successful. In 2014-04-18 CT Scan of the Lungs prompted: bilateral main pulmonary artery thrombosis, so we add a diagnosis pulmonary embolism,we began to give him thrombolytic t herapy. Alteplase 50mg qdnow the INR is 1.95.discharge diagnosis: 1.thrombus of right lower extremity veins 2. pulmonary embolism 3.epididymitis(left)∙Comments:1. No smoking and drinking and keep diet, don’t walk too much, don’t’ sit for a long time.2.Medicines to improve coagulation function ,keep INR 2~3:warfarin 2.5 pills qn.∙ 3. Follow-up clinic visit after one week。
出院小结英文1、英文出院小结Discharge RecordPatient ID:0168220Name: XXXXAge:73-y-o Sex: Male/FemaleAdmissi on Date: XXXXOperati on Date: XXXXDischarge Date: XXXXDiag no sis:Acute myocardial in fracti on...... R CA completely b locked...... L CA has a 50% leisio n in the proximal a nd LAD has 30-50% leisio nsType 2 diabetes mellitus( 2-DM).Admissi on: Sudde n chest pain for 4 hoursPatie nt History: 73-year-old man without sig nifica nt heart problems prese nted with sudde n chest pain for 4 hours. And the pain con sta ntly radiated to the shoulder and back..The electrocardiogram(ECG) of the patie nt showed the ST segment of the leads n ,川,AVF raisedevaluati on mv and was admitted for further and treatme ntCardiovascular Riskfactors: 2-DM, FatPhysical Exam in ati on: Blood pressure 120/60mmHg, Pulse 60/ l ungs were clear. The heart rate was regular, 60 beats per minute. No murmur and pericardial rub was heard. The abdome n was un remarkable. There was no peripheral edema.Laboratory Results:Hb: 133g/L Glucose: mmol/L(<CHOL: L TG: mmol/L LDL-C: mmol/L HDL: mmol/LCRP: L (0-8 mg/L)CK-MB: U/L (0-16 U/L) Tropo nin I: ml (< n g/ml)ECG: a normal rhythm at rate of 60/minute, ST segment raised mv in leads n, m ,AVF.Tran sthoracic Echocardiogram(TTE):The size of left atrium is and the other chamberswere :51%/ \CAG: The middle of right coronary artery(RCA) completely blocked and left cor onary artery (LCA) has a 50% leisi on in the proximal and left an terior desce ndin g(LAD) has some 30-50% leisio ns. After admissi on, we impla nt one stent.15 mm) in the RCA..Treatme nt: After operati on, trearme nt was started for the recovery .It wastreated with Aspirin 100mg po qd , Plavix 75mgpo qd, Dilatrend bid, Imdur 60mg qd, and Clexa ne(low-molecular-weight hepari ns sodium)5000 Usc q12h.. After 16 days of recovery , the patie nt is well. So we thi nk the patie nt can discharge hospital.Medicati on:to improve heart fun cti on and their usesAspiri n 100mg po 1-0-0Plavix 75mg po 1-0-0 for 9 mon thsZocor(statin) 40mg po 0-0-1Micardis 40mg po 1-0-0Spiro nolacto ne 20mg po 1-0-0Dilatre nd po 1-0-1to con trol blood sugar and their usesGlargine(insulin) 34U ih 1-0-0Glucobay 50mg po 1-1-1Avan dia 8mg po 1-0-0Comme nts:1. No smok ing and dr inking and keep diet2. Strictly con troll blood sugar3. Be atte nti on to keep rest and do not do high-i nten sity exercises4. Eat medic in es on time and follow-up visit after one mon th.Dotor: XXXXXX2、英文出院小结姓名Zhao XX 性别male 年龄51入院诊断Acute pancreatitis简要病史、体格检查和入院辅助检查Complai nts:'left upper abdomi nal pa in for 1day.' alcohol triggered. severe, constant pain with nausea & vomiting. moreintense when supine, but relieved by staying with the trunk flexed and kneesdraw n up. no radiati on. no abdo minal diste nti on. no gallst one history. Physical exam in ati on: low-grade fever. no rmal to elevated BP. distressed, an xious.jaundice(-). moderate abdominal tenderness, with no muscle rigidity. Laboratorydata: serum amylase T ,serum lipase T ,urine amylase T ,white blood cells T , plasma glucose T . CTplaint scan: no indicative sign. gastroduodenal endoscopy: inflammatory changes, no ulcer observed. etc.治疗经过:fasting. intravenous fluids. nutritional support. nasogastric suction. prophylactic an tibiotic. in hibit ing pan creatic secreti on. others in cludi ng con sultati ons.出院转归:resoluti on of abdo minal pai n出院诊断:Acute pan creatitis出院医嘱:avoidanee of alcohol. fluid diet gradually to regular diet. symptoms observati on. hospitalizati on whe n n ecessary.3、英文出院小结DICHARGE SUMMARYDISCHARGE DIAGNOSIS1. Un stable angina.2. Multi-vessel artery diease3. HyperlipidemaREASON FOR ADMISSIONis a 69-year-old Chin ese man who is actually a n ative of Beshi ng and in theUnited States visiting his daughter. he presented to the Heart Hospital emergencyroom with substernal discomfort radiating to the arm. There was mild improvementwith nitroglycerin. He had discomfort on and off over a two-day period. He was admitted for further man ageme nt.HOSPITAL COURSEruled out for a myocardial infarction by serial enzymes. An adenosine Cardiolite stress was performed. This showed an terior and in ferior ischemia. Caridiac catheterizati on was the n performed by Dr. Picone. Coronary arteriography revealed a subtotal proximal LAD followed by total occlusi on mid vessel. The distal LAD filled via collaterals from the circumflex and looked small and diffusely diseased. The circumflex was pate nt. There was a 50 perce nt ste no sis in the obtuse margin al. The right coronary artery had a 75 perce nt mid vessel ste no sis and a 100 perce nt distal occlusi on. There were right to right and leftto right collaterals. Left ven triculography revealed an ejection fract ion of55 perce nt with an terior hypok in esis. Dr. Picone felt that he was not an ideal can didate for bypass surgery and recomme nded medical man ageme nt. was started on a comb in ati on of Imdur and metoprolol. Aspiri n was continu ed. On April 26,20XX,he was still having low chest discomfort. It is difficult to get a complete story as the patient is Chinese speaking only. His daughter interpreted.I spent long periods with the family and describing the procedures and what was done and their implicati ons. They will n eed to return to see in two to three he has more chest discomfort, then he may require surgical intervention.DISCHARGE MEDICATIONSMedications on discharge are Imdur 60 mg 25 mg 40 mg 325 mg Norvasc mg up with in two to three weeks.4、出院小结n ame: 巴图吉亚age: 34 sex: man medical record nu mber: 628848 date of admissi on: of discharge: physicia n: zha ngche ngpingprese nt history:8 years ago,he felt jaun dice with no in due ing factors , he first con suited local hospital,blood laboratories tests showed HBsAg is positive,diagnosised as hepatitis B was given for treatment,and the liver function becomed year ago,he was given interferon for treatment after injection 2 times,the treatment stopedfor higher ALT tha n last year,he has take n in termitte ntly pain in the upper abdomen after the further treatment,he admitted to the liver disease toadmission,he has examined liver function and other laboratories.(the result oftest:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L).hospital course:after the patie nt's hostitalizati on ,he was started on heparolysate 100mg 舒肝宁注射液)30ml compound glycyrrhizin 160mg jiaonang(五酯胶囊)jianpiyishen keli(健脾益肾颗粒)10g responded very well to the to now,he changes for the better and no obvious un comfortable.Laboratory data:ALT U/L,AST U/L,total bilirubin umol/L,total protein g/L,albumin g/L.White cell coun t ,hemoglob in ,hematocrit ,platelet coun t ,PT ,AFP mg/ml.admitti ng diag nosis:viral hepatitis with HBVdischarge diag nosis:hepatitis B infection.cirrhosis(mild).Con titi on ondischarge:Stable.discharge in struct ions: diet:home diet.Activity:as tolerated.Discharge Medicati ons:Con ti nued:jiaonang(五酯胶囊)yishen keli(健脾益肾颗粒)10g keli (茵枝黄颗粒)6g follow upup blood routine,prothrombin time(PT),liver function and a-fetoprotein(AFP) in 1 mon th. up HBV-marker,HBV-DNA,AFP and liver ultraso nograph every 6 mon th..sig nature:5、出院小结(外科)Medical CertificateName:——sex: male age:24 in patie nt number: -----In patie nt date: from ,20XX to ,20XXDiag no sis:portal hyperte nsion, liver cirrhosisCourse of treatme nt: First, we had a thorough exam in ati on for this patie nt, in cludi ng physical exam in ati on, blood exam in ati on and image exam in ati on (All the data men ti oned above had bee n copied by the patie nt).The n we had the diag no sis: portal hyperte nsion, liver cirrhosis. And, in ,20XXwe un derwe nt the operati on: sple nectomy with esophagus tran sect ion and an astomosis, and esophagogastric devascularizati on. After operati onthe patie nt had got a basic recovery and was discharged on ,20XX.In structio ns:work. is suggested that he should rest for one month at homebefore resuming hisdoctor and have some n ecessary exam in ati on regularly.doctor any time whe n feeli ng un comfortable.Doctor in charge: Professor ----------20XX-10-9。